This is one of the main reasons I don't take statins anymore. I believe that inflammation is the real problem needing to be solved. Less cholesterol in the bloodstream only means there is less junk to be accreted to the arterial walls. They aren't even solving the correct problem.
Use the labels in the right column to find what you want. Or you can go thru them one by one, there are only 27,739 posts. Searching is done in the search box in upper left corner. I blog on anything to do with stroke.DO NOT DO ANYTHING SUGGESTED HERE AS I AM NOT MEDICALLY TRAINED, YOUR DOCTOR IS, LISTEN TO THEM. BUT I BET THEY DON'T KNOW HOW TO GET YOU 100% RECOVERED. I DON'T EITHER, BUT HAVE PLENTY OF QUESTIONS FOR YOUR DOCTOR TO ANSWER.
Changing stroke rehab and research worldwide now.Time is Brain! trillions and trillions of neurons that DIE each day because there are NO effective hyperacute therapies besides tPA(only 12% effective). I have 523 posts on hyperacute therapy, enough for researchers to spend decades proving them out. These are my personal ideas and blog on stroke rehabilitation and stroke research. Do not attempt any of these without checking with your medical provider. Unless you join me in agitating, when you need these therapies they won't be there.
What this blog is for:
My blog is not to help survivors recover, it is to have the 10 million yearly stroke survivors light fires underneath their doctors, stroke hospitals and stroke researchers to get stroke solved. 100% recovery. The stroke medical world is completely failing at that goal, they don't even have it as a goal. Shortly after getting out of the hospital and getting NO information on the process or protocols of stroke rehabilitation and recovery I started searching on the internet and found that no other survivor received useful information. This is an attempt to cover all stroke rehabilitation information that should be readily available to survivors so they can talk with informed knowledge to their medical staff. It lays out what needs to be done to get stroke survivors closer to 100% recovery. It's quite disgusting that this information is not available from every stroke association and doctors group.
Monday, June 30, 2014
Statins are a mess: we need better data, and shared decision making
An editorial in the British Medical Journal. What does your doctor think?
This is one of the main reasons I don't take statins anymore. I believe that inflammation is the real problem needing to be solved. Less cholesterol in the bloodstream only means there is less junk to be accreted to the arterial walls. They aren't even solving the correct problem.
This is one of the main reasons I don't take statins anymore. I believe that inflammation is the real problem needing to be solved. Less cholesterol in the bloodstream only means there is less junk to be accreted to the arterial walls. They aren't even solving the correct problem.
Advances in Neuromotor Stroke Rehabilitation
It's only 71 pages long, you can see if your doctor and stroke center are using any of these.
http://scholar.google.com/scholar_url?hl=en&q=http://downloads.hindawi.com/journals/specialissues/501651.pdf&sa=X&scisig=AAGBfm1z3jTYqqLSrIUBg4l8fd0Qa2-lkw&oi=scholaralrt
http://scholar.google.com/scholar_url?hl=en&q=http://downloads.hindawi.com/journals/specialissues/501651.pdf&sa=X&scisig=AAGBfm1z3jTYqqLSrIUBg4l8fd0Qa2-lkw&oi=scholaralrt
Reviews of Textbooks of Motor Learning and Neuroplasticity
Does your doctor know about and understand neuroplasticity well enough to get you to 100% recovery? Why the hell not? It is only $39.99.
http://journals.lww.com/jnpt/Citation/2014/07000/Reviews_of_Textbooks_of_Motor_Learning_and.9.aspx

http://journals.lww.com/jnpt/Citation/2014/07000/Reviews_of_Textbooks_of_Motor_Learning_and.9.aspx

Plasma 1,8-cineole correlates with cognitive performance following exposure to rosemary essential oil aroma
Is your hospital room infused with rosemary? Is this nothing more than Pavlovian response? Or placebo?
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3736918/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3736918/
Abstract
Objective
The
mode of influence of the aromas of plant essential oils on human
behaviour is largely unclear. This study was designed to assess the
potential pharmacological relationships between absorbed 1,8-cineole
following exposure to rosemary aroma, cognitive performance and mood.
Methods
Twenty
healthy volunteers performed serial subtraction and visual information
processing tasks in a cubicle diffused with the aroma of rosemary. Mood
assessments were made pre and post testing, and venous blood was sampled
at the end of the session. Pearson correlations were carried out
between serum levels of 1,8-cineole, cognitive performance measures and
change in mood scores.
Results
Here
we show for the first time that performance on cognitive tasks is
significantly related to concentration of absorbed 1,8-cineole following
exposure to rosemary aroma, with improved performance at higher
concentrations. Furthermore, these effects were found for speed and
accuracy outcomes, indicating that the relationship is not describing a
speed–accuracy trade off. The relationships between 1,8-cineole levels
and mood were less pronounced, but did reveal a significant negative
correlation between change in contentment and plasma 1,8-cineole levels.
Conclusion
These
findings suggest that compounds absorbed from rosemary aroma affect
cognition and subjective state independently through different
neurochemical pathways.
Aromas of rosemary and lavender essential oils differentially affect cognition and mood in healthy adults
This has only been out for 11 years, has your doctor included this in your stroke protocol to help your memory and mood? I'd have to see the actual research details before I believe this is not just placebo or recognition by participants that they got the real thing..
Aromas of rosemary and lavender essential oils differentially affect cognition and mood in healthy adults
Abstract
This
study was designed to assess the olfactory impact of the essential oils
of lavender (Lavandula angustifolia) and rosemary (Rosmarlnus
officinalis) on cognitive performance and mood in healthy volunteers.
One hundred and forty-four participants were randomly assigned to one of
three independent groups, and subsequently performed the Cognitive Drug
Research (CDR) computerized cognitive assessment battery in a cubicle
containing either one of the two odors or no odor (control). Visual
analogue mood questionnaires were completed prior to exposure to the
odor, and subsequently after completion of the test battery. The
participants were deceived as to the genuine aim of the study until the
completion of testing to prevent expectancy effects from possibly
influencing the data. The outcome variables from the nine tasks that
constitute the CDR core battery feed into six factors that represent
different aspects of cognitive functioning. Analysis of performance
revealed that lavender produced a significant decrement in performance
of working memory, and impaired reaction times for both memory and
attention based tasks compared to controls. In contrast, rosemary
produced a significant enhancement of performance for overall quality of
memory and secondary memory factors, but also produced an impairment of
speed of memory compared to controls. With regard to mood, comparisons
of the change in ratings from baseline to post-test revealed that
following the completion of the cognitive assessment battery, both the
control and lavender groups were significantly less alert than the
rosemary condition; however, the control group was significantly less
content than both rosemary and lavender conditions. These findings
indicate that the olfactory properties of these essential oils can
produce objective effects on cognitive performance, as well as
subjective effects on mood.
2nd Annual International Translational Nanomedicine (ITNano) Conference has been set for July 25 - 27th
Every decent stroke association and stroke hospital should be attending to figure out how to get drugs thru the blood brain barrier so when we finally get some useful neuoplasticity and neurogenesis drugs we will have a way to deliver them.
http://www.northeastern.edu/itnano/
Northeastern University in Boston July 25 to 27th, 2014.
http://www.northeastern.edu/itnano/
Northeastern University in Boston July 25 to 27th, 2014.
Effects of upper limb robot-assisted therapy on motor recovery in subacute stroke patients
So this is helpful. Whom is going to contact all the PMR doctors and neurologists to make sure this gets included in all stroke protocols within the next month? ASA/NSA are you up to doing some actual work instead of just putting out lazy press releases? That means contacting all of these persons directly. It also means documenting the exact protocols being used so every survivor can see them and make sure their doctor and therapist is using the correct one.
Effects of upper limb robot-assisted therapy on motor recovery in subacute stroke patients
Patrizio Sale1*, Marco Franceschini1, Stefano Mazzoleni23, Enzo Palma1, Maurizio Agosti4 and Federico Posteraro35
Journal of NeuroEngineering and Rehabilitation 2014, 11:104
doi:10.1186/1743-0003-11-104
Published: 19 June 2014
Published: 19 June 2014
Abstract
Background and purpose
There is little evidence available on the use of robot-assisted therapy in subacute
stroke patients. A randomized controlled trial was carried out to evaluate the short-time
efficacy of intensive robot-assisted therapy compared to usual physical therapy performed
in the early phase after stroke onset.
Methods
Fifty-three subacute stroke patients at their first-ever stroke were enrolled 30 ± 7 days
after the acute event and randomized into two groups, both exposed to standard therapy.
Additional 30 sessions of robot-assisted therapy were provided to the Experimental
Group. Additional 30 sessions of usual therapy were provided to the Control Group.
The following impairment evaluations were performed at the beginning (T0), after 15
sessions (T1), and at the end of the treatment (T2): Fugl-Meyer Assessment Scale (FM),
Modified Ashworth Scale-Shoulder (MAS-S), Modified Ashworth Scale-Elbow (MAS-E), Total
Passive Range of Motion-Shoulder/Elbow (pROM), and Motricity Index (MI).
Results
Evidence of significant improvements in MAS-S (p = 0.004), MAS-E (p = 0.018) and pROM
(p < 0.0001) was found in the Experimental Group. Significant improvement was demonstrated
in both Experimental and Control Group in FM (EG: p < 0.0001, CG: p < 0.0001) and
MI (EG: p < 0.0001, CG: p < 0.0001), with an higher improvement in the Experimental
Group.
Conclusions
Robot-assisted upper limb rehabilitation treatment can contribute to increasing motor
recovery in subacute stroke patients. Focusing on the early phase of stroke recovery
has a high potential impact in clinical practice.
Sunday, June 29, 2014
Physical Activity and Exercise Recommendations for Stroke Survivors AHA/ASA Scientific Statement
This is absolutely f*cking appalling. It takes until 2014 to come up with this! Have you all been doing absolutely nothing to figure out how survivors recover for the last 30 years? Only 23 pages. I won't be reading this because I don't need the stress produced by reading drivel. Your doctor should be conversant in everything here.
http://stroke.ahajournals.org/content/early/2014/05/20/STR.0000000000000022.full.pdf+html
http://stroke.ahajournals.org/content/early/2014/05/20/STR.0000000000000022.full.pdf+html
Annually, 795,000 people in the United States experience a stroke; or ≈
1 person every 40 seconds, and nearly one quarter of these strokes are recurrent.
1
An estimated 7 million American adults are living with a stroke,
1
and it is projected that an additional 4 million will have a stroke by 2030, which
is almost a 25% increase in prevalence from 2010.
2
Data from the Framingham Study revealed a lifetime stroke risk of 1 in 5 for women and 1 in 6 for men among those 55 to 75 years of age.
3
Moreover, the incidence of stroke is likely to continue to escalate because of an expanding population of
elderly Americans
4
and the apparent epidemic in the general population regarding modifiable cardiovascular risk factors,
including diabetes mellitus, obesity, and physical inactivity. American adults with disability are more likely to be obese, to smoke, and to be physically inactive,
5
which leads to an increased cardiovascular risk in an already functionally compromised population. When considered independently from other cardiovascular diseases (CVDs), stroke continues to be the fourth-leading cause of death in the United States.
1
Unfortunately, stroke remains a leading cause of long-term disability in the United States.
1
Consequently, stroke survivors are often deconditioned and predisposed to a sedentary lifestyle that adversely impacts performance of activities of daily living, increases the risk for falls, and may contribute to a heightened risk for recurrent stroke and other CVDs. The majority of studies have investigated ischemic stroke, although stroke is often considered a broader term for a transient ischemic attack (TIA), ischemic stroke, or intracerebral hemorrhage. All 3 of these categories pose an increased risk for a future vascular event
6,7
; however, this risk is further elevated in patients with cerebrovascular disease and comorbid CVD.
6,7
Although stroke survivors vary in their level of participation in
physical activity, hospital- and community-based studies have
consistently found low levels of activity.
8,9
On a population basis, the physical activity of community-living stroke survivors is lower than that of older adults with other chronic health conditions of the musculoskeletal or cardiovascular system.
10
Physical activity and exercise have the potential to positively influence multiple physical and psychosocial domains
after stroke. We define physical activity as “any bodily movement produced by skeletal muscles that results in energy
expenditure,” whereas exercise is “a subset of physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness.”
11
There is strong evidence that exercise after stroke can improve cardiovascular fitness,
12
walking ability,
13
and upper-extremity muscle strength.
14
There are less consistent reports of lower-extremity muscle strength gains.
15
Although exercise has been shown to reduce falls in older adults,
16
this finding has not been confirmed in stroke,
17
likely a consequence of too few studies with relatively small sample sizes. Although exercise has primarily been used to improve physical function after stroke, emerging research suggests that exercise may improve depressive symptoms,
18
some aspects of executive functioning and memory,
19–21
and health-related quality of life
22
after stroke and poststroke fatigue.
23
Therefore, stroke survivors can benefit from counseling on increasing participation in physical activity,
24
as well as the appropriate prescription for exercise training. However, most healthcare professionals have limited experience and guidance in exercise programming for this diverse and escalating patient population. The present scientific statement is intended to help bridge the current knowledge gap in physical activity
and exercise recommendations in the stroke population.
The Vibrator Play or In The Next Room
Went to this at a local theater with a bunch of friends. Lots of double entendres but no raunchiness. Play was set in 1880s.
My OT used a vibrator on my arm muscles to get them to fire in the first weeks.
The synopsis here:
In the Next Room or the vibrator play is a comedy about marriage, intimacy, and electricity.
Set in the 1880s at the dawn of the age of electricity and based on the bizarre historical fact that doctors used vibrators to treat 'hysterical' women (and some men), the play centers on a doctor and his wife and how his new therapy affects their entire household.
In a seemingly perfect, well-to-do Victorian home, proper gentleman and scientist Dr. Givings has innocently invented an extraordinary new device for treating "hysteria" in women (and occasionally men): the vibrator. Adjacent to the doctor's laboratory, his young and energetic wife tries to tend to their newborn daughter—and wonders exactly what is going on in the next room. When a new "hysterical" patient and her husband bring a wet nurse and their own complicated relationship into the doctor's home, Dr. and Mrs. Givings must examine the nature of their own marriage, and what it truly means to love someone.
My OT used a vibrator on my arm muscles to get them to fire in the first weeks.
 |
| The antique vibrator |
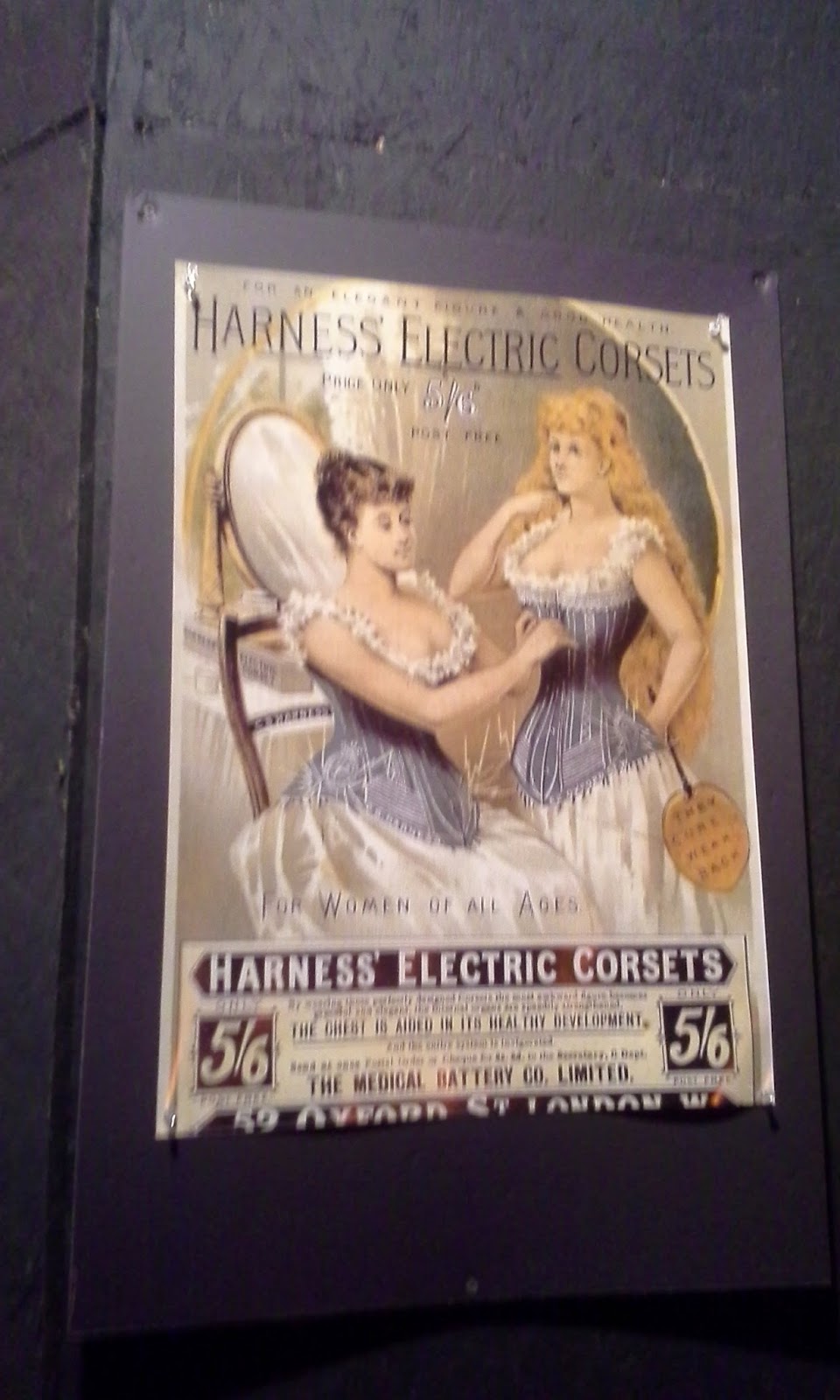 |
| Advertising sign |
 |
| 1906! |
 |
| Advertising sign |
 |
| Advertising sign |
 |
| Advertising sign |
 |
| Center of set - living room |
 |
| right side of set - doctors office |
In the Next Room or the vibrator play is a comedy about marriage, intimacy, and electricity.
Set in the 1880s at the dawn of the age of electricity and based on the bizarre historical fact that doctors used vibrators to treat 'hysterical' women (and some men), the play centers on a doctor and his wife and how his new therapy affects their entire household.
In a seemingly perfect, well-to-do Victorian home, proper gentleman and scientist Dr. Givings has innocently invented an extraordinary new device for treating "hysteria" in women (and occasionally men): the vibrator. Adjacent to the doctor's laboratory, his young and energetic wife tries to tend to their newborn daughter—and wonders exactly what is going on in the next room. When a new "hysterical" patient and her husband bring a wet nurse and their own complicated relationship into the doctor's home, Dr. and Mrs. Givings must examine the nature of their own marriage, and what it truly means to love someone.
Saturday, June 28, 2014
The Scientific Method
I wish our stroke associations would at least take the first step by enumerating all the problems in the stroke world. Doing background research is so damned simple even a stroke-addled survivor like me has been doing if for 5 years.
From http://www.sciencebuddies.org

From http://www.sciencebuddies.org

Proper Rehabilitation Sequence Enables Paralyzed Rats to Regain Grip
This is so f*cking simple and yet no one is going to do this for future human stroke survivors. What exactly should be the protocol for humans?
Ask you doctor exactly what the growth-promoting drugs are so you can determine how YOU want to handle this. Your doctor will do nothing because this is currently not standard of care. The hell with my doctor, if this is a standard drug already approved for human use and minimal side effects, I will have a screaming match with my doctor. It's my brain I'm trying to save and I don't think my doctor has any damn clue on how to do that.
http://www.ptproductsonline.com/2014/06/proper-rehabilitation-sequence-enables-paralyzed-rats-regain-grip/
Ask you doctor exactly what the growth-promoting drugs are so you can determine how YOU want to handle this. Your doctor will do nothing because this is currently not standard of care. The hell with my doctor, if this is a standard drug already approved for human use and minimal side effects, I will have a screaming match with my doctor. It's my brain I'm trying to save and I don't think my doctor has any damn clue on how to do that.
http://www.ptproductsonline.com/2014/06/proper-rehabilitation-sequence-enables-paralyzed-rats-regain-grip/
Researchers from the University of
Zurich, ETH Zurich and the University of Heidelberg demonstrated with an
experiment on rats that a course of therapy that combines the stimulation of
nerve fiber growth with drugs and motor training could improve motor skills.
According to a University of Zurich news release, the research team found that
the key is the correct sequence: paralyzed animals can only make a complete
recovery if the training is delayed until after the growth-promoting drugs have
been administered. The timing, dosage, and type of rehabilitation must be
correct for motor functions to make an almost full recovery after a stroke.
The study was conducted by an
interdisciplinary team headed by Professor Martin Schwab from the Brain
Research Institute at the University of Zurich and ETH Zurich’s Neuroscience
Center. The results of the study showed that the rats paralyzed down one side
by a stroke almost managed to regain their motor functions fully if they were
given the ideal combination of rehabilitative training and substances that
boosted the growth of nerve fibers.
The animals with stroke whose front
legs were paralyzed underwent physical training—specifically, gripping food
pellets. All of the rats in the study received antibody treatment first to
boost nerve-fiber growth and motor training. The results revealed that for
those who began later training , they regained 85% of their original motor
skills. For the rats trained straight after stroke in parallel with the
antibodies, physical performance in the grip test remained very low at 15%.
The University of Zurich news
release indicates that anatomical studies have confirmed the importance of the
right rehabilitation schedule: depending on the therapeutic design, different
patterns of new nerve fibers that sprouted into the cervical spinal cord from
the healthy part of the brain and thus aid functional recovery to varying
degrees were apparent.
Study head Martin Schwab states,
“Our study reveals how important a meticulous therapeutic design is for the
most successful rehabilitation possible. The brain has enormous potential for
the reorganization and reestablishment of its functions. With the right
therapies at the right time, this can be increased in a targeted fashion.”
First author of the study
Anna-Sophia Wahl says, “This new rehabilitative approach at least triggered an
astonishing recovery of the motor skills in rats, which may become important
for the treatment of stroke patients in the future.”
Rehabilitation Goal Setting: Theory, Practice and Evidence
Your doctor better be reading this book right now and comparing what s/he is doing for their stroke patients to this. It's only $121.40, One of your visits pays for it.
http://books.google.com/books?id=HaThAwAAQBAJ&printsec=frontcover#v=onepage&q&f=false

http://books.google.com/books?id=HaThAwAAQBAJ&printsec=frontcover#v=onepage&q&f=false

PTSD Awareness Day: The Future of Treatment
Come on Dana Foundation I expected more of you. No mention of marijuana as a treatment for PTSD. I'm sure they have hundreds of employees and they can't keep up-to-date on research involving PTSD or at least know how to use Google Scholar. GAH!!!!!
http://danablog.org/2014/06/27/ptsd-awareness-future-of-treatment/
http://danablog.org/2014/06/27/ptsd-awareness-future-of-treatment/
A long-term, complex, unitary appraisal regarding neurorestorative, including neurorehabilitative, outcomes in patients treated with Cerebrolysin®, following traumatic brain injury
You'll have to ask your doctor if Cerebrolysin® is going to be added to their stroke protocol.
A long-term, complex, unitary appraisal regarding neurorestorative, including neurorehabilitative, outcomes in patients treated with Cerebrolysin®, following traumatic brain injury
Authors: Daia CO, Haras M, Spircu T, Anghelescu A, Onose L, Ciurea AV, Mihăescu AS, Onose G
Published Date June 2014
Volume 2014:2 Pages 85 - 93
DOI: http://dx.doi.org/10.2147/JN.S49693
| Received: |
30 December 2013 |
|---|---|
| Accepted: | 20 February 2014 |
| Published: | 26 June 2014 |
1Carol Davila University of Medicine and Pharmacy, Bucharest, Romania; 2Bagdasar-Arseni Teaching Emergency Hospital, Bucharest, Romania; 3Metrorex – The Medical Service, Bucharest, Romania
Background: Neuroprotection is a modern therapeutic concept that has some useful outcomes discussed in the literature, including for traumatic brain injury (TBI).
Scope and study design: This was a retrospective case-control study that was approved by the bioethics commission of the Bagdasar-Arseni Teaching Emergency Hospital, Bucharest, Romania. The aim of the study was to comparatively assess neurorestorative, including neurorehabilitative, outcomes obtained with or without Cerebrolysin®.
Materials and methods: Nineteen cases treated with Cerebrolysin versus 28 who did not receive this drug were included in this study. All cases had a subacute or post-acute status after TBI and were hospitalized (only at their first admission) between January 2005 and December 2010 in the hospital's NeuroRehabilitation Clinic Division. Epidemiological, clinical, paraclinical, and functional parameters were evaluated, using the: Functional Independence Measure (FIMTM), Glasgow Outcome Score (GOS), and Modified Rankin Scale.
Results: Patients in the Cerebrolysin group had, on average, higher (although not statistically significant) FIM evolution values (36.53) than the control group (29.64) (P=0.174, 95% confidence interval: -8.0 to 21.8). The effect size assessed on the GOS was 2.1%. Additionally, the mean FIM value at admission of the Cerebrolysin group (45.79) was lower than that of controls (61.50; P=0.076).
Discussion and conclusion: The clinical/functional evolution, comparatively evaluated in the studied inpatients, and taking into account the small sample and effect sizes – including for GOS – suggest that Cerebrolysin, correctly indicated and administered, may perhaps contribute to some improvement of post-TBI patients' overall neurorestorative/rehabilitative outcomes; this given the short period (approximately 1 month) over which the medicine's action was evaluated, the lower FIM mean value at admission in the Cerebrolysin group, and respectively that, for severe central nervous system lesions – including after TBI – and consequent conditions, it cannot yet be concluded that any therapeutic approaches, such as Cerebrolysin, can significantly improve post-injury outcomes.
Keywords: neuroprotection, Functional Independence Measure (FIM), brain trauma
Blocking key enzyme minimizes stroke injury
Whom is following this with human clincal trials?
http://www.utsouthwestern.edu/newsroom/news-releases/year-2014/june/stroke-bibb.html
A drug that blocks the action of the enzyme Cdk5 could substantially reduce brain damage if administered shortly after a stroke, UT Southwestern Medical Center research suggests.
The findings, reported in the June 11 issue of the Journal of Neuroscience, determined in rodent models that aberrant Cdk5 activity causes nerve cell death during stroke.
“If you inhibit Cdk5, then the vast majority of brain tissue stays alive without oxygen for up to one hour,” said Dr. James Bibb, Associate Professor of Psychiatry and Neurology and Neurotherapeutics at UT Southwestern and senior author of the study. “This result tells us that Cdk5 is a central player in nerve cell death.”
More importantly, development of a Cdk5 inhibitor as an acute neuroprotective therapy has the potential to reduce stroke injury.
“If we could block Cdk5 in patients who have just suffered a stroke, we may be able to reduce the number of patients in our hospitals who become disabled or die from stroke. Doing so would have a major impact on health care,” Dr. Bibb said.
While several pharmaceutical companies worked to develop Cdk5 inhibitors years ago, these efforts were largely abandoned since research indicated blocking Cdk5 long-term could have detrimental effects. At the time, many scientists thought aberrant Cdk5 activity played a major role in the development of Alzheimer’s disease and that Cdk5 inhibition might be beneficial as a treatment.
Based on Dr. Bibb’s research and that of others, Cdk5 has both good and bad effects. When working normally, Cdk5 adds phosphates to other proteins that are important to healthy brain function. On the flip side, researchers have found that aberrant Cdk5 activity contributes to nerve cell death following brain injury and can lead to cancer.
“Cdk5 regulates communication between nerve cells and is essential for proper brain function. Therefore, blocking Cdk5 long-term may not be beneficial,” Dr. Bibb said. “Until now, the connection between Cdk5 and stroke injury was unknown, as was the potential benefit of acute Cdk5 inhibition as a therapy.”
In this study, researchers administered a Cdk5 inhibitor directly into dissected brain slices after adult rodents suffered a stroke, in addition to measuring the post-stroke effects in Cdk5 knockout mice.
“We are not yet at a point where this new treatment can be given for stroke. Nevertheless, this research brings us a step closer to developing the right kinds of drugs,” Dr. Bibb said. “We first need to know what mechanisms underlie the disease before targeted treatments can be developed that will be effective. As no Cdk5 blocker exists that works in a pill form, the next step will be to develop a systemic drug that could be used to confirm the study’s results and lead to a clinical trial at later stages.”
Currently, there is only one FDA-approved drug for acute treatment of stroke, the clot-busting drug tPA. Other treatment options include neurosurgical procedures to help minimize brain damage.
Additional UT Southwestern scientists from the Department of Psychiatry who contributed to this study were lead author and former postdoctoral researcher Dr. Douglas Meyer; postdoctoral researcher Dr. Melissa Torres-Altoro; Instructor Dr. Florian Plattner; and former postdoctoral researcher Dr. Janice Kansy.
The work was supported by grants from the National Institutes of Health. Pharmaceutical company Boehringer Ingelheim provided the Cdk5-inhibiting compound indolinone used in the study.
This work is just one of numerous cutting-edge stroke research studies taking place at UT Southwestern, where patients have access to the newest treatments and clinical trials due in part to the stroke center’s recent Advanced Comprehensive Stroke Center certification. This designation is the highest level of certification for stroke care by The Joint Commission. UT Southwestern’s Robert D. Rogers Advanced Comprehensive Stroke Center offers the most advanced treatment available from a multidisciplinary team of vascular neurologists, endovascular specialists, vascular surgeons, neuro-radiologists and neuro-intensivists who are on call 24 hours a day to treat stroke patients.
For information on UT Southwestern’s certification as an Advanced Comprehensive Stroke Center and our stroke patient outcomes, visit UTSW Medicine.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty includes many distinguished members, including six who have been awarded Nobel Prizes since 1985. Numbering more than 2,700, the faculty is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide medical care in 40 specialties to nearly 91,000 hospitalized patients and oversee more than 2 million outpatient visits a year.
http://www.utsouthwestern.edu/newsroom/news-releases/year-2014/june/stroke-bibb.html
A drug that blocks the action of the enzyme Cdk5 could substantially reduce brain damage if administered shortly after a stroke, UT Southwestern Medical Center research suggests.
The findings, reported in the June 11 issue of the Journal of Neuroscience, determined in rodent models that aberrant Cdk5 activity causes nerve cell death during stroke.
“If you inhibit Cdk5, then the vast majority of brain tissue stays alive without oxygen for up to one hour,” said Dr. James Bibb, Associate Professor of Psychiatry and Neurology and Neurotherapeutics at UT Southwestern and senior author of the study. “This result tells us that Cdk5 is a central player in nerve cell death.”
More importantly, development of a Cdk5 inhibitor as an acute neuroprotective therapy has the potential to reduce stroke injury.
“If we could block Cdk5 in patients who have just suffered a stroke, we may be able to reduce the number of patients in our hospitals who become disabled or die from stroke. Doing so would have a major impact on health care,” Dr. Bibb said.
While several pharmaceutical companies worked to develop Cdk5 inhibitors years ago, these efforts were largely abandoned since research indicated blocking Cdk5 long-term could have detrimental effects. At the time, many scientists thought aberrant Cdk5 activity played a major role in the development of Alzheimer’s disease and that Cdk5 inhibition might be beneficial as a treatment.
Based on Dr. Bibb’s research and that of others, Cdk5 has both good and bad effects. When working normally, Cdk5 adds phosphates to other proteins that are important to healthy brain function. On the flip side, researchers have found that aberrant Cdk5 activity contributes to nerve cell death following brain injury and can lead to cancer.
“Cdk5 regulates communication between nerve cells and is essential for proper brain function. Therefore, blocking Cdk5 long-term may not be beneficial,” Dr. Bibb said. “Until now, the connection between Cdk5 and stroke injury was unknown, as was the potential benefit of acute Cdk5 inhibition as a therapy.”
In this study, researchers administered a Cdk5 inhibitor directly into dissected brain slices after adult rodents suffered a stroke, in addition to measuring the post-stroke effects in Cdk5 knockout mice.
“We are not yet at a point where this new treatment can be given for stroke. Nevertheless, this research brings us a step closer to developing the right kinds of drugs,” Dr. Bibb said. “We first need to know what mechanisms underlie the disease before targeted treatments can be developed that will be effective. As no Cdk5 blocker exists that works in a pill form, the next step will be to develop a systemic drug that could be used to confirm the study’s results and lead to a clinical trial at later stages.”
Currently, there is only one FDA-approved drug for acute treatment of stroke, the clot-busting drug tPA. Other treatment options include neurosurgical procedures to help minimize brain damage.
Additional UT Southwestern scientists from the Department of Psychiatry who contributed to this study were lead author and former postdoctoral researcher Dr. Douglas Meyer; postdoctoral researcher Dr. Melissa Torres-Altoro; Instructor Dr. Florian Plattner; and former postdoctoral researcher Dr. Janice Kansy.
The work was supported by grants from the National Institutes of Health. Pharmaceutical company Boehringer Ingelheim provided the Cdk5-inhibiting compound indolinone used in the study.
This work is just one of numerous cutting-edge stroke research studies taking place at UT Southwestern, where patients have access to the newest treatments and clinical trials due in part to the stroke center’s recent Advanced Comprehensive Stroke Center certification. This designation is the highest level of certification for stroke care by The Joint Commission. UT Southwestern’s Robert D. Rogers Advanced Comprehensive Stroke Center offers the most advanced treatment available from a multidisciplinary team of vascular neurologists, endovascular specialists, vascular surgeons, neuro-radiologists and neuro-intensivists who are on call 24 hours a day to treat stroke patients.
For information on UT Southwestern’s certification as an Advanced Comprehensive Stroke Center and our stroke patient outcomes, visit UTSW Medicine.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty includes many distinguished members, including six who have been awarded Nobel Prizes since 1985. Numbering more than 2,700, the faculty is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide medical care in 40 specialties to nearly 91,000 hospitalized patients and oversee more than 2 million outpatient visits a year.
How our brains store recent memories, cell by single cell
Your doctor should be able to figure out a protocol to solve your short-term memory problems.
http://www.mdlinx.com/internal-medicine/newsl-article.cfm/5344414/ZZF307965849E94474BB34FC062CEC0F93/?
http://www.mdlinx.com/internal-medicine/newsl-article.cfm/5344414/ZZF307965849E94474BB34FC062CEC0F93/?
UC San Diego Health System, 06/17/2014
Confirming what neurocomputational theorists have long suspected,
researchers at the Dignity Health Barrow Neurological Institute in
Phoenix, Ariz. and University of California, San Diego School of
Medicine report that the human brain locks down episodic memories in the
hippocampus, committing each recollection to a distinct, distributed
fraction of individual cells. The findings, published in the June 16
Early Edition of PNAS, further illuminate the neural basis of human
memory and may, ultimately, shed light on new treatments for diseases
and conditions that adversely affect it, such as Alzheimer’s disease and
epilepsy. “To really understand how the brain represents memory, we
must understand how memory is represented by the fundamental
computational units of the brain – single neurons – and their networks,”
said Peter N. Steinmetz, MD, PhD, program director of neuroengineering
at Barrow and senior author of the study. “Knowing the mechanism of
memory storage and retrieval is a critical step in understanding how to
better treat the dementing illnesses affecting our growing elderly
population.”
Cat Stroke Survivor Gets Water Therapy
I bet the cat recovers better than 99% of human stroke survivors.
http://www.myfoxphilly.com/story/25879369/cat-stroke-survivor-gets-water-therapy
http://www.myfoxphilly.com/story/25879369/cat-stroke-survivor-gets-water-therapy
After Stroke, Spouse May Also Need Care
For me it was quite simple. Since I wasn't following therapist instructions to the letter I was not going to recover. My ex had the expectation that all I had to do to recover was follow the therapist instructions. I couldn't disagree because I had no medical background and disagreeing with her was attacking and saying her medical background was not worth listening to. Whoa!
http://health.usnews.com/health-news/articles/2014/06/26/after-stroke-spouse-may-also-need-care
If your spouse has a stroke, and the two of you disagree about the rate of recovery, your own health might suffer, a new study finds.
The caregiving spouse is at increased risk for emotional distress and depression if the couple has different perceptions of the post-stroke progress, researchers found.
Stroke care needs to switch from focusing only on the patient to regarding the patient and spouse as one unit, suggested Michael McCarthy, a social work researcher at the University of Cincinnati.
"How the spouse is doing matters in the equation," McCarthy said.
"They need as much care, if not more in some ways, as the patient," he added. "We need to bring partners together in the rehabilitation process, to align each person's expectations and perceptions in order to achieve the best outcomes."
More at link
http://health.usnews.com/health-news/articles/2014/06/26/after-stroke-spouse-may-also-need-care
If your spouse has a stroke, and the two of you disagree about the rate of recovery, your own health might suffer, a new study finds.
The caregiving spouse is at increased risk for emotional distress and depression if the couple has different perceptions of the post-stroke progress, researchers found.
Stroke care needs to switch from focusing only on the patient to regarding the patient and spouse as one unit, suggested Michael McCarthy, a social work researcher at the University of Cincinnati.
"How the spouse is doing matters in the equation," McCarthy said.
"They need as much care, if not more in some ways, as the patient," he added. "We need to bring partners together in the rehabilitation process, to align each person's expectations and perceptions in order to achieve the best outcomes."
More at link
Five Top Research Advances in Traumatic Brain Injury
For stroke this should be the responsibility of our stroke associations. But they either can't or won't do something like this that is so f*cking simple. I don't have time to compile this for stroke.
http://brainposts.blogspot.com/2014/06/five-top-research-advances-in-traumatic.html
http://brainposts.blogspot.com/2014/06/five-top-research-advances-in-traumatic.html
Friday, June 27, 2014
Understand the worldview of those you're trying to reach - Stroke associations
This line from Seth Godin pretty much encompasses everything that is wrong with most of our stroke associations. Most survivors have a disability they want to overcome and nothing useful is seen to be worked on to understand exactly how neurogenesis and neuroplasticity can be replicated on a consistent basis to get survivors to complete recovery. Yet most communications from our stroke associations is about prevention. Tremendous mismatch there that they don't even recognize. Probably because they have no survivor advisory committee or any survivors in positions of authority. I blame the board of directors for not setting appropriate direction.
Virtual Lobby Days event by the National Stroke Association
This email encompasses all what is wrong with our stroke associations;
No strategic plan, just a scattershot approach. The extremely simple answer is to create a National Stroke Plan like the National Plan to Address Alzheimer’s Disease
or H.R. 1098, the Traumatic Brain Injury Reauthorization (TBI) Act of 2013.
By creating a strategic plan all these activities lead to one result, lower death and disability due to stroke.
But no, we get this crap;
http://www.stroke.org/site/R?i=_BNRNDBD8z9SEdSeL7174g
No strategic plan, just a scattershot approach. The extremely simple answer is to create a National Stroke Plan like the National Plan to Address Alzheimer’s Disease
or H.R. 1098, the Traumatic Brain Injury Reauthorization (TBI) Act of 2013.
By creating a strategic plan all these activities lead to one result, lower death and disability due to stroke.
But no, we get this crap;
http://www.stroke.org/site/R?i=_BNRNDBD8z9SEdSeL7174g
Having trouble? View this message on our website.
 |
|
|
Insect diet helped early humans build bigger brains, study suggests
Is your neurologist having you forage for your food to spur your higher-level cognitive functions? And that low-fat, high-protein diet from this would probably be better than anything you get in the hospital.
http://news.wustl.edu/news/Pages/27058.aspx
Figuring out how to survive on a lean-season diet of hard-to-reach ants, slugs and other bugs may have spurred the development of bigger brains and higher-level cognitive functions in the ancestors of humans and other primates, suggests research from Washington University in St. Louis. “Challenges associated with finding food have long been recognized as important in shaping evolution of the brain and cognition in primates, including humans,” said Amanda D. Melin, PhD, assistant professor of anthropology in Arts & Sciences and lead author of the study.
“Our work suggests that digging for insects when food was scarce may have contributed to hominid cognitive evolution and set the stage for advanced tool use.” Based on a five-year study of capuchin monkeys in Costa Rica, the research provides support for an evolutionary theory that links the development of sensorimotor (SMI) skills, such as increased manual dexterity, tool use, and innovative problem solving, to the creative challenges of foraging for insects and other foods that are buried, embedded or otherwise hard to procure.
Published in the June 2014 Journal of Human Evolution, the study is the first to provide detailed evidence from the field on how seasonal changes in food supplies influence the foraging patterns of wild capuchin monkeys.
The study is co-authored by biologist Hilary C. Young and anthropologists Krisztina N. Mosdossy and Linda M. Fedigan, all from the University of Calgary, Canada.
It notes that many human populations also eat embedded insects on a seasonal basis and suggests that this practice played a key role in human evolution.
“We find that capuchin monkeys eat embedded insects year-round but intensify their feeding seasonally, during the time that their preferred food – ripe fruit – is less abundant,” Melin said. “These results suggest embedded insects are an important fallback food.”
Previous research has shown that fallback foods help shape the evolution of primate body forms, including the development of strong jaws, thick teeth and specialized digestive systems in primates whose fallback diets rely mainly on vegetation.
This study suggests that fallback foods can also play an important role
in shaping brain evolution among primates that fall back on insect-based
diets, and that this influence is most pronounced among primates that
evolve in habitats with wide seasonal variations, such as the wet-dry
cycles found in some South American forests.
“Capuchin monkeys are excellent models for examining evolution of
brain size and intelligence for their small body size, they have
impressively large brains,” Melin said. “Accessing hidden and
well-protected insects living in tree branches and under bark is a
cognitively demanding task, but provides a high-quality reward: fat and
protein, which is needed to fuel big brains.”
But when it comes to using tools, not all capuchin monkey strains and lineages are created equal, and Melin’s theories may explain why.
Perhaps the most notable difference between the robust (tufted, genus Sapajus) and gracile (untufted, genus Cebus) capuchin lineages is their variation in tool use. While Cebus monkeys are known for clever food-foraging tricks, such as banging snails or fruits against branches, they can’t hold a stick to their Sapajus cousins when it comes to the
innovative use and modification of sophisticated tools.
One explanation, Melin said, is that Cebus capuchins have historically and consistently occupied tropical rainforests, whereas the Sapajus lineage spread from their origins in the Atlantic rainforest into drier, more temperate and seasonal habitat types.
“Primates who extract foods in the most seasonal environments are expected to experience the strongest selection in the ‘sensorimotor intelligence’ domain, which includes cognition related to object handling,” Melin said. “This may explain the occurrence of
tool use in some capuchin lineages, but not in others.”
Genetic analysis of mitochondial chromosomes suggests that the Sapajus-Cebus diversification occurred millions of years ago in the late Miocene epoch.
http://news.wustl.edu/news/Pages/27058.aspx
Figuring out how to survive on a lean-season diet of hard-to-reach ants, slugs and other bugs may have spurred the development of bigger brains and higher-level cognitive functions in the ancestors of humans and other primates, suggests research from Washington University in St. Louis. “Challenges associated with finding food have long been recognized as important in shaping evolution of the brain and cognition in primates, including humans,” said Amanda D. Melin, PhD, assistant professor of anthropology in Arts & Sciences and lead author of the study.
“Our work suggests that digging for insects when food was scarce may have contributed to hominid cognitive evolution and set the stage for advanced tool use.” Based on a five-year study of capuchin monkeys in Costa Rica, the research provides support for an evolutionary theory that links the development of sensorimotor (SMI) skills, such as increased manual dexterity, tool use, and innovative problem solving, to the creative challenges of foraging for insects and other foods that are buried, embedded or otherwise hard to procure.
Published in the June 2014 Journal of Human Evolution, the study is the first to provide detailed evidence from the field on how seasonal changes in food supplies influence the foraging patterns of wild capuchin monkeys.
The study is co-authored by biologist Hilary C. Young and anthropologists Krisztina N. Mosdossy and Linda M. Fedigan, all from the University of Calgary, Canada.
It notes that many human populations also eat embedded insects on a seasonal basis and suggests that this practice played a key role in human evolution.
“We find that capuchin monkeys eat embedded insects year-round but intensify their feeding seasonally, during the time that their preferred food – ripe fruit – is less abundant,” Melin said. “These results suggest embedded insects are an important fallback food.”
Previous research has shown that fallback foods help shape the evolution of primate body forms, including the development of strong jaws, thick teeth and specialized digestive systems in primates whose fallback diets rely mainly on vegetation.
But when it comes to using tools, not all capuchin monkey strains and lineages are created equal, and Melin’s theories may explain why.
Perhaps the most notable difference between the robust (tufted, genus Sapajus) and gracile (untufted, genus Cebus) capuchin lineages is their variation in tool use. While Cebus monkeys are known for clever food-foraging tricks, such as banging snails or fruits against branches, they can’t hold a stick to their Sapajus cousins when it comes to the
innovative use and modification of sophisticated tools.
One explanation, Melin said, is that Cebus capuchins have historically and consistently occupied tropical rainforests, whereas the Sapajus lineage spread from their origins in the Atlantic rainforest into drier, more temperate and seasonal habitat types.
“Primates who extract foods in the most seasonal environments are expected to experience the strongest selection in the ‘sensorimotor intelligence’ domain, which includes cognition related to object handling,” Melin said. “This may explain the occurrence of
tool use in some capuchin lineages, but not in others.”
Genetic analysis of mitochondial chromosomes suggests that the Sapajus-Cebus diversification occurred millions of years ago in the late Miocene epoch.
Thursday, June 26, 2014
Traumatic Brain Injury in Veterans May Increase Risk of Dementia
With this and your 33% dementia chance post-stroke from an Australian study. Your doctors should have a defined protocol to prevent that dementia as part of their standard of care.
Good luck finding any doctor who can do something other than the generic crap like;
The generic crap from Harvard
Or pretty much the same crap from Mayo clinic
http://dgnews.docguide.com/traumatic-brain-injury-veterans-may-increase-risk-dementia?
My suggestions are here:
Dementia prevention 19 ways
Good luck finding any doctor who can do something other than the generic crap like;
The generic crap from Harvard
Or pretty much the same crap from Mayo clinic
http://dgnews.docguide.com/traumatic-brain-injury-veterans-may-increase-risk-dementia?
My suggestions are here:
Dementia prevention 19 ways
Hare's Psychopathy Checklist
I'm not bad, only an 11 on the lower side of the bell curve. I was just curious.
The test here:
http://vistriai.com/psychopathtest/
The explanation of the disorder here:
http://www.minddisorders.com/knowledge/Hare_Psychopathy_Checklist.html
Do not read anything into your results, that is for a qualified doctor to administer and decode.
The test here:
http://vistriai.com/psychopathtest/
The explanation of the disorder here:
http://www.minddisorders.com/knowledge/Hare_Psychopathy_Checklist.html
Do not read anything into your results, that is for a qualified doctor to administer and decode.
H.R. 1098, the Traumatic Brain Injury Reauthorization (TBI) Act of 2013.
Stroke has nothing. There are 7 million survivors in the US, adding 500,000 every year. With that and friends/family, we are at least 50 million strong. That's enough to get some decent legislation if we had a great stroke association. We have no useful stroke associations at all, unless you count press releases as useful. Alzheimers has National Plan to Address Alzheimer’s Disease
The TBI one here:
https://www.govtrack.us/congress/bills/113/hr1098
The TBI one here:
https://www.govtrack.us/congress/bills/113/hr1098
Wednesday, June 25, 2014
New research shows almonds reduce the risk of heart disease
How long will it take for your hospital to have almonds added to all stroke survivors diets? 10?, 15? 20 years? Or never? Do they even have a post-stroke diet plan? Mine here;
Research found that they significantly increase the amount of antioxidants in the blood stream, reduce blood pressure and improve blood flow. These findings add weight to the theory that Mediterranean diets with lots of nuts have big health benefits.
The study was led by Professor Helen Griffiths, Professor in Biomedical Sciences and Executive Dean of the School of Life and Health Sciences at Aston University in Birmingham, UK. Researchers tested the effects of a short-term almond-enriched diet on healthy young and middle-aged men as well as on a group of young men with cardiovascular risk factors including having high blood pressure or being overweight. A control group ate what they normally would, while another group consumed snacks of 50g of almonds a day for one month.
At the end of the study period, the group eating an almond-enriched diet had higher levels of antioxidants (alpha-tocopherol) in their blood stream, improved blood flow and lower blood pressure, potentially reducing their risk of heart disease.
Almonds are known to contain a range of beneficial substances such as vitamin E and healthy fats, fibre which increases the sense of fullness, and flavonoids which may have antioxidant properties. The team believes it is likely to be the combination of all these nutrients working together to create the overall health benefits rather than just one particular nutrient in isolation.
Professor Griffiths said: “Our study confirms that almonds are a superfood. Previous studies have shown that they keep your heart healthy, but our research proves that it isn’t too late to introduce them into your diet - adding even a handful (around 50g) every day for a short period can help. You could replace a daytime snack with a bag of almonds or add them to your regular meals like porridge or muesli to help reduce your risk of heart problems.”
What would a post-stroke diet look like per Dean?
http://www.aston.ac.uk/about/news/releases/2014/june/research-show-almonds-reduce-risk-of-heart-disease/Research found that they significantly increase the amount of antioxidants in the blood stream, reduce blood pressure and improve blood flow. These findings add weight to the theory that Mediterranean diets with lots of nuts have big health benefits.
The study was led by Professor Helen Griffiths, Professor in Biomedical Sciences and Executive Dean of the School of Life and Health Sciences at Aston University in Birmingham, UK. Researchers tested the effects of a short-term almond-enriched diet on healthy young and middle-aged men as well as on a group of young men with cardiovascular risk factors including having high blood pressure or being overweight. A control group ate what they normally would, while another group consumed snacks of 50g of almonds a day for one month.
At the end of the study period, the group eating an almond-enriched diet had higher levels of antioxidants (alpha-tocopherol) in their blood stream, improved blood flow and lower blood pressure, potentially reducing their risk of heart disease.
Almonds are known to contain a range of beneficial substances such as vitamin E and healthy fats, fibre which increases the sense of fullness, and flavonoids which may have antioxidant properties. The team believes it is likely to be the combination of all these nutrients working together to create the overall health benefits rather than just one particular nutrient in isolation.
Professor Griffiths said: “Our study confirms that almonds are a superfood. Previous studies have shown that they keep your heart healthy, but our research proves that it isn’t too late to introduce them into your diet - adding even a handful (around 50g) every day for a short period can help. You could replace a daytime snack with a bag of almonds or add them to your regular meals like porridge or muesli to help reduce your risk of heart problems.”
Linking Executive Control and Emotional Response A Training Procedure to Reduce Rumination
This sounds exactly like what survivors need to stop focusing on negative thoughts. What protocol is your doctor creating to solve this problem? And if you had less damage because your doctor had prevented the neuronal cascade of death I bet you would be less likely to focus on negative thoughts.
http://cpx.sagepub.com/content/early/2014/04/28/2167702614530114.abstract
http://cpx.sagepub.com/content/early/2014/04/28/2167702614530114.abstract
- 1Department of Psychology and the Zlotowski Center for Neuroscience, Ben-Gurion University of the Negev
- 2School of Education, Hebrew University of Jerusalem
- Noga Cohen, Department of Psychology, Ben-Gurion University of the Negev, P.O.B. 653, Beer-Sheva 84105, Israel E-mail: nogac@post.bgu.ac.il
- Nilly Mor, School of Education, Hebrew University, Mount Scopus, Jerusalem 91905, Israel E-mail: nilly.mor@mail.huji.ac.il
-
Author Contributions N. Cohen and N. Mor developed the experimental design. Data collection was performed by N. Cohen and by three undergraduate research assistants. Data analysis was performed by N. Cohen under the supervision of N. Mor. The article was drafted by N. Cohen and N. Mor and A. Henik provided critical revisions. All authors approved the final version of the article for submission.
Abstract
Rumination, a maladaptive self-reflection,
is a risk factor for depression, thought to be maintained by executive
control
deficits that impair ruminators’ ability to ignore
emotional information. The current research examined whether training
individuals
to exert executive control when exposed to negative
stimuli can ease rumination. A total of 85 participants were randomly
assigned to one of two training conditions. In the
experimental condition activation of executive control was followed
predominantly
by the presentation of negative pictures, whereas
in the control condition it was followed predominantly by neutral
pictures.
As predicted, participants in the experimental
group showed reduced state rumination compared with those in the control
group.
Furthermore, trait rumination, and particularly its
maladaptive subtype brooding, was associated with increased sadness
only
among participants in the control group, and not in
the experimental group. We argue that training individuals to exert
executive
control when processing negative stimuli can
alleviate ruminative thinking and rumination-related sad mood.
Tuesday, June 24, 2014
Framework for rehabilitation decisions after stroke - 1997 version
From a 1997 article in Stroke magazine.
http://stroke.ahajournals.org/content/28/7/1522.full
------------------------------------------------------------------------------------------------------------
Australia at least has these:
Acute Stroke Services Framework
------------------------------------------------------------------------------------------------------------
I can't find anything newer so you'll have to ask your doctor;
What is your framework for getting me to 100% recovery?
Lets analyze;
1. Nothing on what to do if the patient is not able to learn. Damn it you give them cognitive training.
2. No questions on fatigue
2. Nothing on what the doctor should be doing - other than letting millions of neurons die during the first week due to the neuronal cascade of death.
This is fucking pathetic even for 17 years ago. And for this crap you are actually paying your doctor?

http://stroke.ahajournals.org/content/28/7/1522.full
------------------------------------------------------------------------------------------------------------
Australia at least has these:
Acute Stroke Services Framework
------------------------------------------------------------------------------------------------------------
I can't find anything newer so you'll have to ask your doctor;
What is your framework for getting me to 100% recovery?
Lets analyze;
1. Nothing on what to do if the patient is not able to learn. Damn it you give them cognitive training.
2. No questions on fatigue
2. Nothing on what the doctor should be doing - other than letting millions of neurons die during the first week due to the neuronal cascade of death.
This is fucking pathetic even for 17 years ago. And for this crap you are actually paying your doctor?

FDA warns about blood clot risk with testosterone products
Well your doctor has a lot of studying to do.
Testosterone Improves Woman’s Brain Functions
Testosterone increases neurotoxicity of glutamate in vitro and ischemia-reperfusion injury in an animal model
Thinking with your gonads: testosterone and cognition
Effect of testosterone on functional recovery in a castrate male rat stroke model
Lower Testosterone Levels Predict Incident Stroke and Transient Ischemic Attack in Older Men
Could androgens maintain specific domains of mental health in aging men by preserving hippocampal neurogenesis?
FDA warns about blood clot risk with testosterone products
“Replacing” a hormone the body normally makes when it is running low isn’t necessarily the safest thing to do. Women and their doctors learned this with estrogen after menopause. Now the FDA is sounding a warning that testosterone therapy can cause potentially dangerous blood clots in men.Blood clots that form in veins (what doctors call venous thromboembolism) come in two “flavors.” Deep-vein thrombosis, or DVT, is a blood clot that forms in a deep vein, often in the leg. It can make the affected leg swell or cause leg pain. If a DVT, or part of one, breaks away and gets into the bloodstream, it can block blood flow to the lungs. This is called a pulmonary embolism. A large pulmonary embolism can be deadly. Pulmonary embolism, along with DVT, kill as many as 180,000 Americans each year, more than the number of people who die from breast, prostate, colon, and skin cancers combined.
The FDA had previously warned about a testosterone-therapy-related increase in blood clots in men with a condition called polycythemia. Polycythemia is a condition in which the body makes too many red blood cells, which increases the risk of blood clots. Its latest warning comes from reports of blood clots in men without polycythemia.
The new warning is not related to the FDA’s evaluation of possible links between testosterone therapy and stroke, heart attack, and death.
More at link.
Gradually Increased Training Intensity Benefits Rehabilitation Outcome after Stroke by BDNF Upregulation and Stress Suppression
I'm sorry but I think there is a different reason for the better recovery. Neurogenesis generated by exercise.
http://scholar.google.com/scholar_url?hl=en&q=http://downloads.hindawi.com/journals/bmri/2014/925762.pdf&sa=X&scisig=AAGBfm16QdPV8a9IIoYq7c3V1YmHPhYqAA&oi=scholaralrt
http://scholar.google.com/scholar_url?hl=en&q=http://downloads.hindawi.com/journals/bmri/2014/925762.pdf&sa=X&scisig=AAGBfm16QdPV8a9IIoYq7c3V1YmHPhYqAA&oi=scholaralrt
Rehabilitation for post-stroke cognitive impairment: an overview of recommendations arising from systematic reviews of current evidence
Well these lazy bastards, in the last paragraph they throw up their hands in defeat.
Why not try these? Are you that incompetent that you don't keep up and read current research?
Are you waiting for someone else to propose something? All the while your stroke patients are not getting better. Current standard of care for stroke is a complete failure yet no one wants to create something new.
Why not try these? Are you that incompetent that you don't keep up and read current research?
Are you waiting for someone else to propose something? All the while your stroke patients are not getting better. Current standard of care for stroke is a complete failure yet no one wants to create something new.
The Myths, Realities, and Ethics of Neuroenhancement
Inside the Strange New World of DIY Brain Stimulation
The Art and Science of Cognitive Rehabilitation Therapy
Six Take-aways on Neuroplasticity and Cognitive training By: Dr. Son Preminger
Video Game Training Improves Cognitive Control in Older Adults
Video game training enhances cognitive control in older adults
Towards a Smart Population: A Public Health Framework for Cognitive Enhancement
Want to Slow Mental Decay? Play a Video Game
Reading Cartoons Good for Your Health
APP-titude: Apps for Brain Injury Rehab
http://cre.sagepub.com/content/early/2014/06/18/0269215514538982.abstract
- 1Clinical Neuropsychology Service, Western General Hospital, Edinburgh, UK
- 2Stroke Research, University of Manchester, Manchester, UK
- 3Department of Occupational Therapy, NHS Fife, Fife, UK
- 4Retired, UK
- 5Department of Health Sciences, University of York, York, UK
- 6Nursing, Midwifery and Allied Health Professions Research Unit, Glasgow Caledonian University, Glasgow, UK
- David C Gillespie, Clinical Neuropsychology Service, Department of Clinical Neurosciences (DCN), Western General Hospital, Edinburgh EH4 2XU, UK. Email: david.gillespie@nhslothian.scot.nhs.uk
Abstract
Background: Although
cognitive impairments are common following stroke, there is considerable
uncertainty about the types of interventions
that can reduce activity restrictions and
improve quality of life. Indeed, a recent project to identify priorities
for research
into life after stroke determined that the top
priority for patients, carers and health professionals was how to
improve cognitive
impairments.
Objective: To provide an overview of the evidence for the effectiveness of cognitive rehabilitation for patients with stroke and to
determine the main gaps in the current evidence base.
Methods: Evidence was synthesised for the six Cochrane reviews relating to rehabilitation for post-stroke cognitive impairment and
any subsequently published randomized controlled trials to February 2012.
Results: Data arising
from 44 trials involving over 1500 patients was identified. Though there
was support for the effectiveness of
cognitive rehabilitation for some cognitive
impairments, significant gaps were found in the current evidence base.
All of
the Cochrane reviews identified major
limitations within the evidence they identified.
Conclusions: There is
currently insufficient research evidence, or evidence of insufficient
quality, to support clear recommendations
for clinical practice. Recommendations are made
as to the research required to strengthen the evidence base, and so
facilitate
the delivery of effective interventions to
individuals with cognitive impairment after stroke.
Subscribe to:
Posts (Atom)
 and
and