Yep, but that includes social connections at bars for jazz and trivia. Which is verboten by research in the Lancet. I am vastly blessed by the number of friends I have after getting divorced and moving to Michigan. Life is great.
Safest level of alcohol consumption is none, worldwide study shows
The latest here:
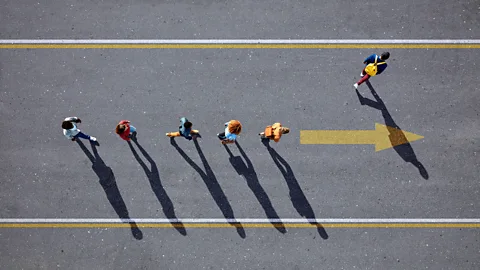
Want to live a long life? Start prioritising your friends
Your social network may influence your health as much as your exercise routine. David Robson, the author of a new book about our relationships, explores the evidence and reasons for this surprising link.
If you have paid attention to the latest thinking on wellbeing and longevity, you will have noticed increasing focus on the state of our relationships. People with thriving social networks, we are told, tend to be far healthier than those who feel isolated.
Our interactions with others are so strongly linked to our longevity that the World Health Organization has just founded a new Commission on Social Connection, calling it "a global health priority".
You may be a little sceptical about these claims, and the mysterious mechanisms that are supposed to tie our physical wellbeing with the strength of our relationships. But our understanding of the "biopsychosocial" model of health has been growing for decades. While investigating the science for my book The Laws of Connection, I discovered that our friendships can influence everything from our immune system's strength to our chances of dying from heart disease.
The conclusions of this research are clear: if we want to live a long and healthy life, we should start prioritising the people around us.
The roots of the science can be traced to the early 1960s. Back then, Lester Breslow at the California State Department of Public Health set out on an ambitious project to identify the habits and behaviours that led to greater longevity. To do so, he recruited nearly 7,000 participants from the surrounding Alameda County. Through comprehensive questionnaires, he built an extraordinarily detailed picture of their lifestyles, and then tracked their wellbeing over the subsequent years.
Take part
A BBC study about your friendships
We'd like to hear about your own relationships, and the ways that they might be changing in the 21st Century. To take part in our anonymous study about friendship, complete this short questionnaire we've designed with the help of psychologist Ian MacRae. You'll learn more about your relationships in a personalised report, and help inform results that we'll publish on BBC.com later this year.
Within a decade, Breslow's team had identified many of the ingredients that we now know are essential for good health: don't smoke; drink in moderation; sleep seven to eight hours a night; exercise; avoid snacks; maintain a moderate weight; eat breakfast. At the time, the findings were so striking that when his colleagues presented the results to him, he believed they were playing some kind of prank. You will hardly need me to explain these guidelines in more detail – the "Alameda 7" are now the basis of most public health guidance.
The research continued, however, and by 1979, two of Breslow's colleagues – Lisa Berkman and S Leonard Syme – had discovered an eighth factor that influenced people's longevity: social connection. On average, the people with the greatest number of ties were around half as likely to die as the people who had smaller networks. The result remained even after they had controlled for factors such as socioeconomic status and people's health at the survey's start, as well as cigarette consumption, exercise and diet.
 Getty Images
Getty ImagesDelving deeper, it became clear that all kinds of relationships mattered, but some were more meaningful than others. A sense of connection with spouses and close friends offered the greatest protection, but even casual acquaintances at church or a bowling club helped to stave off the grim reaper.
The sheer audacity of the claim may explain why it was initially neglected in public health guidance. Scientists were used to seeing the body as a kind of machine, largely detached from our mental state and our social environment. But since then, extensive research has confirmed that connection and loneliness influence our susceptibility to many diverse diseases.
The heart of the matter
Social support can boost your immune system and protect you from infection, for instance. In the 1990s, Sheldon Cohen at Carnegie Mellon University in the US asked 276 participants to give full details of their social ties. They were tested for an existing infection, then placed in quarantine and asked to inhale water droplets laced with rhinovirus – the bug behind many coughs and sneezes. Over the following five days, many of the participants went on to develop symptoms, but this was significantly less likely if they had a large and diverse range of social connections. Indeed, those with the lowest levels of social connection had three to four times the risk of developing a cold than those with richer networks of family, friends, colleagues and acquaintances.
Any good scientist should always consider whether other confounding factors might explain the result. It's reasonable to assume that lonely people could be less fit and active, for example, if they spend less time out and about with friends and family. As Berkman and Syme had also discovered, however, the link remained even after the researchers accounted for all those factors. And the size of the effect vastly exceeds the benefits of popping vitamin supplements – another measure we might take to boost our immune system.
 Getty Images
Getty ImagesThe social health boost extends to our risk of chronic, life-changing conditions such as type 2 diabetes. This arises when the pancreas stops producing enough insulin, and the body's cells stop responding to the insulin that's flowing through the blood – both of which prevent it from breaking down blood sugar to power cells. Factors such as obesity can contribute to diabetes, but so, it seems, does the quality of your relationships. A study of 4,000 participants in the English Longitudinal Study of Ageing found that a higher score on the UCLA Loneliness Scale – a questionnaire that scientists use to measure social connection – predicted the onset of type 2 diabetes over the following decade. There are even signs that people with stronger social ties have a reduced risk of developing Alzheimer's disease and other forms of dementia.
The strongest evidence, however, concerns cardiovascular diseases. Massive studies tracking the health of tens of thousands of people over many years have repeatedly highlighted the link. This can be seen in the earliest stages – people with poor social relationships are more likely to develop hypertension – and in the worst outcomes, with loneliness increasing the risk of a heart attack, angina or stroke by about 30%.
To get a measure of the social health boost's overall importance, Julianne Holt-Lunstad, a psychologist at Brigham Young University, in Provo, Utah, compiled the findings of 148 studies. Together they covered 300,000 participants and had looked at the benefits of social integration and the hazard of social disconnection. She then compared the effects of loneliness with the risks of various other lifestyle factors, including smoking, drinking alcohol, exercise and physical activity, body mass index (a measure of obesity), air pollution and taking medication to control blood pressure.
The results, published in 2010, were astonishing: Holt-Lunstad found that the size and quality of people's social relationships either equalled or outmatched almost all the other factors in determining people's mortality. The more people feel supported by the people around them, the better their health and the less likely they were to die. Overall, social connection – or its absence – played a larger role in people's health than alcohol consumption, exercise, body mass index and air pollution. Only the effects of smoking came close.
Correlation or causation?
This research has faced critics. For iron-clad proof of a causal link between one lifestyle factor and overall longevity, you'd need to conduct a controlled experiment, in which you randomly allocate people to different conditions. That's how new medicines are tested – some take the pill and others take a placebo, and you then record the different outcomes. In this case, you would have to allocate some people to a loneliness condition, denying them friendships, while others are given a ready-made social network full of loving people. Clearly, this is ethically dubious and practically impossible to do – a fact that has led some people to question whether the apparent effects of social connection are real and significant. They suggest that the scientists might have missed some confounding factor that gives the illusion of a link between our social lives and our health and longevity, despite their best efforts.
 Getty Images
Getty ImagesThis argument isn't quite as damning as it seems, however, as Holt-Lunstad recently argued in a review of the research. After all, we can't conduct randomised experiments on humans to prove the life-shortening dangers of smoking – the ethics would be even more problematic – but few scientists today would deny the fact that the one causes the other. That's because scientists have other criteria – known as the Bradford Hill guidelines – to demonstrate a causal link between a lifestyle and a disease.
Holt-Lunstad points out that in long-term studies such as the Alameda research, for example, scientists can look for "temporality" – whether someone's lifestyle choice precedes the development of illness. In this case, the sequence is very clear: the people reported their loneliness long before they developed their ill health. Scientists can also look for a "dose–response relationship" – whether greater exposure of the proposed lifestyle factor results in greater risk. Once again, there is a clear pattern – someone who is completely isolated is more likely to suffer worse health than someone who is occasionally lonely, who in turn suffers more illness than someone who has a vibrant social circle.
You can also check whether the findings are consistent across different populations and using different measurement types. If the effects have only been identified in one small sample, or if they only appear when you consider a single loneliness questionnaire, you would be right to be sceptical. But this is not the case.
The social health boost has also now been documented across the world, says Holt-Lunstad, using multiple methods to quantify people's social connections. Whether you are asking for subjective feelings or considering objective facts, such as someone's marital status or the exact number of times they see acquaintances each month, the pattern stays the same. We can even see parallel effects in other social species as diverse as dolphins, chacma baboons and rhesus macaques: the more integrated an individual is within its group, the greater its longevity.
Safety in numbers
To understand how and why the strength of our social ties could influence our health to such a degree, we must consider our evolution. As early humans adapted to living in bigger groups, everything from food supply to protection from predators would have depended on their relationships. To lose standing with companions would have left them in danger of starvation, illness and injury.
 Getty Images
Getty ImagesAs a result, the brain and body may have evolved to interpret social isolation as a serious threat. This could be the reason we feel such anguish when we are lonely and disconnected. In much the same way that physical pain warns us to seek out safety and tend to our wounds, social pain may have evolved to persuade us to avoid hostile parties and reestablish our positive relationships.
Feelings of rejection or seclusion also set off a cascade of physiological reactions. In our evolutionary past, these were supposed to protect early humans from the immediate danger posed by isolation, such as attacks from predators or enemies. The brain triggers the release of norepinephrine and cortisol – hormones that keep the mind alert to threats and prepares the body for aggression. The immune system, meanwhile, starts ramping up the production of inflammatory molecules to defend from pathogens. For early humans, this would have reduced the risk of infection if they happened to be injured by an attack. A sense of isolation and social stress can also increase the creation of fibrinogen. This promotes blood clotting and would have helped wounds to heal.
While this response would have increased our chances of short-term survival for our ancestors, it can cause longer-term damage. When the body is constantly prepared for hostility and aggression, it puts extra strain on the cardiovascular system. Chronic inflammation, meanwhile, may prevent wound infection, but the accompanying immune response is less adept at responding to viruses – which would increase the chances of catching a respiratory illness, for example. Chronic inflammation also causes wear and tear on our other cells that can raise the risk of diabetes, Alzheimer's and heart disease. The elevated levels of the clotting factor fibrinogen, meanwhile, can cause thrombosis, which may lead to a heart attack or stroke.
If we spend decades in loneliness and isolation, these changes can drastically raise the risk of illness and early death. When people enjoy connection and social support, however, their bodies will suppress processes such as inflammation. As a result, they will have a much better baseline of health that renders them less susceptible to disease.
As someone who has suffered from shyness, I once found these findings a little disconcerting. How can we reap the benefits of deep connection if we are not naturally gregarious and extroverted? But as I have delved into the evidence, I have discovered that our social skills are like our muscles – the more we use them, the stronger they become. Even self-declared introverts can learn to be more sociable, if they wish.
In much the same way that we plan a fitness regime to boost our physical activity, we can all find ways to integrate more meaningful social interaction in our lives, nurturing old bonds and building new ones. We are wired to connect, if only we provide ourselves with the right opportunities.
* This is an edited extract from the book The Laws of Connection: The Scientific Secrets of Building a Strong Social Network, by David Robson. He is @d_a_robson on X and @davidarobson on Instagram and Threads.
TAKE PART IN A BBC.COM STUDY: We'd like to learn more about your friendships and relationships. If you have five minutes, complete this short anonymous questionnaire and receive a personalised report about your how you interact with others in conversation. We'll analyse and publish the results on BBC.com later this year.


