Well, useless, you don't tell us what this wearable self-balancing exoskeleton
robot is so we can direct our doctors to get it. How fucking stupid are you?
Application of Novel Wearable Self-Balancing Exoskeleton Robot Capable for Complete Self-Support in Post-stroke Rehabilitation: A Case Study
Published: July 04, 2024
DOI: 10.7759/cureus.63831
Cite this article as: Zhang Y, Li Z, Zhang Y, et al. (July 04, 2024) Application of Novel Wearable Self-Balancing Exoskeleton Robot Capable for Complete Self-Support in Post-stroke Rehabilitation: A Case Study. Cureus 16(7): e63831. doi:10.7759/cureus.63831
Abstract
Early weight-bearing and trunk control training are essential components for promoting lower limb motor recovery in individuals with stroke. In this case study, we presented the successful implementation of a three-week wearable self-balancing exoskeleton robot training program for a 57-year-old male patient who had suffered from a stroke. After carefully reviewing the patient's previous medical records, conducting a thorough assessment, and excluding other potential contraindications, we introduced wearable self-balancing exoskeleton robot training to complement conventional rehabilitation in managing balance and lower limb function. The training program included early initiation of weight bearing and trunk control training following an ischemic stroke, aimed at promoting motor recovery and improving functional independence. The findings indicated that training with a wearable self-balancing exoskeleton robot enhanced the balance and motor function of the hemiplegic patient, with commendable adherence. Furthermore, the participants consistently reported increased satisfaction and confidence during the training sessions. This case report not only provided preliminary evidence of the effectiveness of the wearable self-balancing exoskeleton robot in promoting functional recovery following a stroke but also outlined a comprehensive training program that may hold value for future clinical application.
Introduction
Walking problems occur in up to 80% of persons post-stroke, and it is reported that 70% of individuals with stroke are at risk for falling [1]. Enhancing the quality of life and promoting psychological well-being for stroke survivors relies on achieving safe, independent, effective, and efficient real-world mobility. This not only improves functional independence but also fosters self-reliance [2].
The 2016 American Heart Association/American Stroke Association Guideline recommends robot-assisted movement training to improve motor function after stroke as class IIb-level A evidence [3], and it is also endorsed as level A evidence by the 2019 Canadian Stroke Best Practice Recommendations [4]. One meta-analysis shows that patients with severe lower limb impairment post-stroke demonstrate better outcomes in terms of walking movements and daily activities when they receive robot-assisted rehabilitation [5]. With the assistance of a robot, many recommended training, such as early initiation of weight-bearing, integration of trunk and limb activities, controllable balance training, and attainment of a symmetrical gait pattern, can be feasibly implemented with high dosage and prolonged duration [6]. The use of robot training conserves significant therapist resources and reduces the time for participants to commence recovery, potentially enabling individuals with latent capabilities to achieve their maximum potential for rehabilitation.
The self-balancing exoskeleton robot is an innovative technology that enables participants’ weight-bearing training even in the stage of paralysis. It can also elicit protective reactions to maintain balance when shifting the center of gravity, thereby promoting the restoration of trunk balance control function. Furthermore, with this technology, therapists can now focus on therapeutic intervention while minimizing falling risks. A user satisfaction study recruited a group of seven individuals with physical disabilities and found that the self-balancing exoskeleton robot demonstrated superior ease of transfer compared to other robotic devices [7], thus offering significant rehabilitation opportunities for persons with severely impaired locomotor function.
Currently, while the effectiveness of robots in lower limb stroke rehabilitation has been recognized; however, the actual application modalities in clinical practice vary, and there is a lack of training programs with sufficient details. Therefore, this case study aims to demonstrate the utilization of wearable self-balancing exoskeleton robots in the balance and lower limb function rehabilitation of stroke patients, with a specific focus on its clinical application methods and clinical efficacy. This case report adheres to the CAse REport (CARE) guidelines.
Case Presentation
Patient information
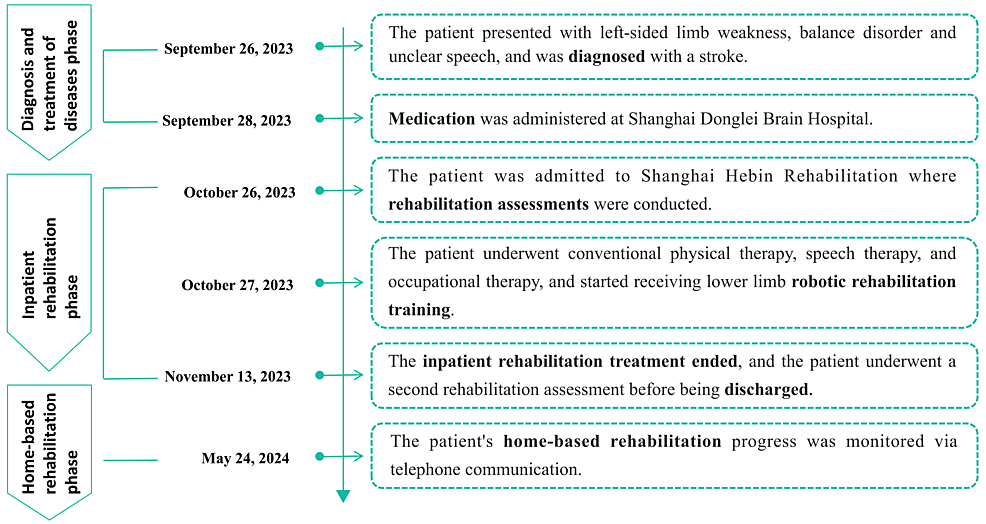
A 57-year-old male was admitted to the rehabilitation hospital due to left-sided weakness, balance disorder, and slurred speech one month ago on September 26, 2023. After being diagnosed with an ischemic stroke (infarction in the right centrum semiovale and genu of corpus callosum, as well as bilateral subcortical lacunar infarctions), he received drug treatment in the hospital, including clopidogrel bisulfate tablets, atorvastatin calcium tablets, and other medications to improve and circulation and restore cerebral perfusion. Although his condition stabilized after the acute phase of stroke treatment, the movement disorder still significantly impacted his daily life. The patient was capable of sitting independently but required assistance for standing, walking, and performing basic self-care tasks, which caused significant distress. The patient had a 20-year history of diabetes but achieved acceptable blood glucose control with subcutaneous insulin and oral metformin. He does not have any significant family medical history or orthopedic conditions, joint diseases, or other complications. Moreover, the patient demonstrated clear consciousness without any cognitive impairment and exhibited the ability to comprehend and successfully execute medical staff instructions. He received conventional physical therapy, speech therapy, and occupational therapy subsequently. The patient was informed by the rehabilitation therapist about the availability of a wearable self-balancing exoskeleton robot that could provide a stable standing support platform to promote the recovery of balance and lower limb function. Recognizing the potential benefits, the patient proactively chose this treatment method on October 27, 2023, driven by a strong desire for prompt recovery (Figure 1).
Clinical findings
The Brunnstrom recovery stage assessment showed that the patient's left upper limb, hand, and lower limb were classified as stage III, stage III, and stage II, respectively. The hemiplegic limbs did not show spasticity, and the Modified Ashworth Scale (MAS) score was 0. The simplified three-level balance assessment method revealed that the patient exhibited a level 2 sitting balance (capable of sustaining dynamic balance for over three seconds, accompanied by upper limb movement) and a level 0 standing balance (incapable of maintaining static self-balance for more than three seconds). In daily life, the patient heavily relied on wheelchairs for his activities. The patient reported no pain during daily activities and rehabilitation treatment. The patient exhibited hyporeflexia and positive pathological reflexes or hyper-reflexia in the affected lower limb (Table 1). The patients had normal body size, with 168 cm height and 66 kg weight. The assessment results of the active and passive range of motion in the upper and lower limbs were presented in Table 2, indicating that the patient fulfilled the fundamental criteria for undergoing robotic training.
More at link, maybe you can guess from the pictures there.
No comments:
Post a Comment