If your doctor and hospital WERE COMPETENT AT ALL, they would have created a protocol on exoskeletons already from all this earlier research! But since they are TOTALLY FUCKING INCOMPETENT, THEY HAVE DONE NOTHING!
Interim results of exoskeletal wearable robot for gait recovery in subacute stroke patients
- Article
- Open access
- Published:
Scientific Reports volume 15, Article number: 11671 (2025)
Abstract
Exoskeletons have been proposed for potential clinical use to improve ambulatory function in patients with stroke. The aim of an interim analysis of an international, multicenter, randomized, controlled trial was to investigate the short-term effect of overground gait training using a torque-assisted exoskeleton in subacute stroke patients with severe ambulatory functional impairment. Data from a total of 93 subacute stroke patients with severe ambulatory functional impairment were analyzed. All participants received a total of 20 sessions; five sessions per week for 4 weeks. The robot-assisted gait training (RAGT) group received 30 min of conventional gait training and 30 min of gait training using an exoskeleton (ANGEL LEGS M20, Angel robotics, Co., Ltd.), while the control group received 60 min of conventional gait training. Functional assessments were conducted before and immediately after the final intervention by a rater blinded to group assignment. Overground gait training with a torque-assisted exoskeleton in this study showed improvement in gait function comparable to conventional gait rehabilitation in subacute stroke patients, with additional gains in lower extremity strength. These findings suggest that the overground gait training with a torque-assisted exoskeleton might be a potential intervention for subacute stroke patients.
Clinical Trial Registration: NCT05157347 (the first registration (10/12/2021)).
Introduction
The restoration of ambulatory function in stroke patient is a critical goal in rehabilitation, as ambulation plays a key role in determining the patient’s ability to perform activities in their home and social environment1. In the acute stroke phase, approximately 80% of patients have ambulatory impairment. Despite recovery of ambulatory function within the first six months after stroke onset, many patients do not fully regain their pre-stroke mobility2. Therefore, facilitating earlier and more pronounced improvement in ambulatory function for the purpose of stroke rehabilitation is of considerable importance.
There has been considerable research into the efficacy of robotic gait rehabilitation3. The use of a robot can facilitate the practice of correct and repetitive movements by patients with the necessary amount and intensity of training4. To date, the majority of robotic gait rehabilitation techniques used in stroke rehabilitation have been treadmill-based robots designed to facilitate control of the gait cycle3. However, the conditions of treadmill-based robotic gait training differ from those of actual overground gait. Consequently, the improvement in gait ability following treadmill-based robotic training may not directly correlate with improved overground gait5. In addition, the use of a robot to control locomotion may present challenges in adapting robotic movements to the patient’s effort to activate muscles and to the passive characteristics of the musculoskeletal system6. The use of an exoskeleton for above-ground gait training has been proposed as a means to promote activation of the nervous system, with the aim of inducing active participation by the patient to facilitate active balance control, weight shift and muscle activation6. Recently, several exoskeletons have been proposed for potential clinical use with the aim of supporting functional ambulation in patients who have suffered a stroke6,7,8,9.
We are currently conducting an international, multi-center study to determine the effect of overground gait training with a torque-assisted exoskeleton on the recovery of ambulatory function in patients with subacute stroke (ClinicalTrial.gov, NCT05157347, 15/12/2021)10. During the trial, interim analyses were conducted to verify the safety and short-term effectiveness of the study. Although the clinical trial is still ongoing, preliminary results from the interim analyses have yielded remarkable results that we would like to present in this report. The analysis in subacute stroke patients with severe ambulatory functional impairment, where gait training by a therapist is difficult, has not been reported in previous studies. The aim of this interim report was to investigate the short-term effect of overground gait training using a torque-assisted exoskeleton in subacute stroke patients with severe ambulatory functional impairment.
Results
Participant characteristics.
Data from a total of 93 participants randomized into two groups (47 in the robot-assisted gait training (RAGT) group and 46 in the control group) were analyzed in this interim study. Twelve subacute stroke patients in the RAGT group (25.5%) withdrew during the intervention for various reasons; new major illness unrelated to the intervention (n = 3), desire to stop (n = 7), less than 80% of the training session (n = 1) and other personal reasons (n = 1). Six subacute stroke patients in the control group (13.0%) withdrew during the intervention because they wanted to stop (n = 2) and for other personal reasons (n = 4). The dropout rate in the RAGT group tended to be higher than in the control group without statistical significance (p = 0.189). However, there were no notable adverse effects observed in either the RAGT or control groups as a result of the intervention, including an increase in spasticity, falls, or fractures. Finally, 75 participants (35 in the RAGT group and 40 in the control group) completed the 4-week intervention and were included in the interim analysis (Fig. 1).
Table 1 shows the baseline characteristics of the RAGT and control groups. There was no significant difference in baseline characteristics between the RAGT and control groups. There was no significant difference in ambulation, motor function, balance function and functional independence between the two groups at T0. There was also no significant difference in mood and quality of life between the two groups at T0. In addition, the supplementary table shows the comparison of baseline characteristics between participants who completed the intervention and those who dropped out in the RAGT group. There was no significant difference in all baseline characteristics between participants who completed the intervention and those who dropped out in the RAGT group (Supplementary Table S1).
Change in behavioral assessments
Ambulatory function
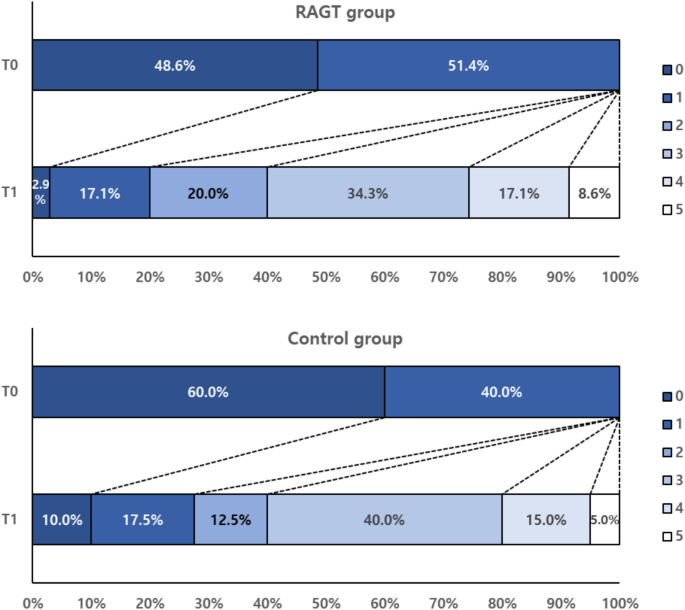
Figure 2 illustrates the shift in Functional Ambulatory Category (FAC) among participants in each RAGT and control group. There was a significant improvement in FAC from T0 to T1 in each RAGT and control group (p < 0.05). In the RAGT group, 80.0% of participants had a FAC greater than or equal to 2, while 72.5% of the control group had a FAC greater than or equal to 2. However, no statistically significant difference was observed in the shift of FAC between the two groups.
Motor and balance function
There was a significant improvement in the leg score in the Motricity Index (MI-LL) from T0 to T1 in each the RAGT and control group (p < 0.05). MI-LL at T1 was significantly higher in the RAGT group than in the control group (p = 0.025 with post-hoc power = 0.745). In addition, hip flexion, knee extension, and ankle dorsiflexion strength showed significantly greater improvements in the RAGT group than in the control group (p = 0.042 with post-hoc power = 0.658, p = 0.043 with post-hoc power = 0.646, and p = 0.032 with post-hoc power = 0.693, respectively, Table 2).
There was a significant improvement in BBS from T0 to T1 in each RAGT and control group (p < 0.05). However, there was no significant difference in BBS at T1 between the two groups (Table 2).
Functional independence
There was a significant improvement in Functional Independence Measure (FIM) from T0 to T1 in each RAGT and control group (p < 0.05). However, there was no significant difference in FIM at T1 between the two groups (Table 2).
Mood and quality of life
There was a significant improvement in Geriatric Depression Scale-short form (GDS-SF) and Euro Quality of Life (EQ)-5D from T0 to T1 in each RAGT and control group (p < 0.05). However, there was no significant difference in GDS-SF and EQ-5D between the two groups at T1 (Table 2).
Discussion
The results of this interim analysis showed that the overground gait training with a torque-assisted exoskeleton for 4 weeks could improve ambulatory function to the same extent as conventional physical therapy. In addition, the overground gait training with an exoskeleton might provide the additional motor functional improvement with safety in subacute stroke patients with severe ambulatory impairment.
The overground gait training with an exoskeleton in this study did yield any significant adverse effects over a 4-week period in subacute stroke patients. These findings, in conjunction with the effects and safety of previous robot-assisted gait training3,4,11, indicate that overground gait training with a torque-assisted exoskeleton used in this study was comparable to conventional physical therapy for improvement of ambulatory function in subacute stroke patients. In particular, given that the subjects in this study required significant physical assistance from the physical therapist for gait training with FAC 0 or 1, the results of this study confirm the advantages of robot-assisted rehabilitation, which can reduce the physical burden on the therapist. These results are expected to serve as a basis for the clinical use of robot-assisted gait training in the future.
In addition to an improvement in gait function, this study demonstrated an enhancement in the MI-LL. MI-LL refers to the improvement of lower limb muscle strength12. In this study, we found that both proximal and distal lower limb muscle strength were significantly increased in comparison to the control group. MI-LL is recognized as a key variable in enhancing walking function in subacute stroke patients13,14. The augmented strength gains observed in the RAGT cohort relative to the control group in this study might facilitate the improvement of walking function following the continuation of rehabilitation. This interim analysis will be substantiated upon the completion of the full study trial and the subsequent analysis of the results. It is probable that the additional strength gains observed in the RAGT group in this study were attributable to the nature of the wearable robot. The use of robot-assisted walking devices has been shown to result in a reduction in lower limb muscle activity during ambulation in stroke15. However, the exoskeleton in this study was designed to facilitate assistance in accordance with the patient’s specific torques, which were automatically detected by a ground contact sensor, encoders in the actuators, and an inertial measurement unit sensor located in a backpack. Consequently, it incorporated a resistance exercise component that demanded more muscle strength.
The efficacy of RAGT in enhancing lower limb strength in stroke patients has been previously documented in the literature for treadmill-based exoskeleton robot16, and foot plate-based end-effector devices17. Furthermore, the use of an overground exoskeleton for RAGT has also been demonstrated to be an effective method for improving strength18,19. The incorporation of resistance training into gait training using an overground exoskeleton has been demonstrated to be an effective method for improving strength. The rationale behind this approach may be that the weight-bearing component of conventional rehabilitation could be relatively limited in stroke patients with impaired gait and balance. Consequently, gait training with an overground exoskeleton could facilitate a resistance training component through weight bearing, with a greater duration and intensity than conventional rehabilitation. In particular, in patients with severe ambulatory functional impairment, which were the participants of this study, the therapist had to exert a considerable amount of effort to increase weight bearing, which places a limit on the amount of resistance training that could be provided. The study also found no specific side effects, such as an increase in spasticity or musculoskeletal pain, were observed in the RAGT group. The overground gait training with a torque-assisted exoskeleton employed in this study provides indirect evidence that resistance training in conjunction with functional exercise may prove to be a more efficacious approach.
Goffredo et al.6 previously demonstrated that gait rehabilitation utilizing an overground wearable exoskeleton in subacute stroke patients enhanced gait function and augmented lower limb strength in a single group. However, the absence of a control group in the aforementioned study precludes the determination of its comparative efficacy with conventional gait training. In addition, Zhang et al.20 recently conducted a randomized controlled trial in 24 subacute stroke patients and reported that gait rehabilitation with an overground wearable exoskeleton was effective in improving balance compared to upright bed training. However, the results of this study confirmed the improvement in gait function and increase in lower limb muscle strength in the RAGT group as reported by Goffredo et al.6 and, in particular, showed that the increase in lower limb muscle strength was effective compared to conventional gait rehabilitation. However, this study and previous studies of above-ground wearable exoskeletons have not confirmed the superiority of improving walking function compared to conventional gait rehabilitation, and further research is needed.
There were no significant complications or adverse events in the RAGT and control group of this study. It is probable that this is a consequence of the conservative exclusion criteria employed in the selection of the study population, which included conditions that would be anticipated to present certain challenges in the utilization of the overground wearable exoskeleton. In light of the promising safety profile observed in a limited subacute stroke patient population, further studies are recommended to expand the study population to include a larger number of subacute stroke patients. Although this study demonstrated the stability of the overground wearable exoskeleton in subacute stroke patients, it is notable that the dropout rate in the RAGT group was relatively high. This was a limitation of this study. The predominant reason for withdrawal from the study in the RAGT group was the desire to stop, while no participants in the control group withdrew for this reason. The characteristics of those who withdrew were not significantly different from those who completed the study in RAGT group. Therefore, it could be inferred that RAGT might present a more substantial challenge to stroke patients compared to conventional rehabilitation. In order to provide further substantiation for this interpretation, it would have been advantageous to assess the participants’ motivation for gait rehabilitation in advance. However, this was not feasible, constituting a limitation of the study. Although the study recruited patients with no other functional deficits, the relatively high dropout rate represents a potential limitation of the wearable exoskeleton used in this study. In the future, it would be beneficial to develop application protocols with greater precision in order to facilitate the implementation of gait rehabilitation with an overground wearable exoskeleton for a larger cohort of subacute stroke patients. Additionally, the relatively higher dropout rate observed in the RAGT group in comparison to the control group could be perceived as a potential source of bias in the results of this study. However, given that there were no discernible differences in the characteristics of the completers and dropouts, it can be concluded that the representativeness of the completers is not a significant concern. It should be noted that this study was conducted as an interim analysis, with the number of subjects not predetermined. It is evident that the interim analysis included a sufficient number of subjects and statistical power. However, it is imperative to report the confirmatory results after the completion of the full study. In addition, a number of factors, including cognitive function, have been identified as contributors to the recovery of ambulatory function in stroke patients.14,21 Cognitive function has been identified as a pivotal element in the gait and balance in stroke patients22. Interventions with dual-task training have demonstrated efficacy in enhancing gait and balance function in stroke patients23. Consequently, it is imperative to examine the characteristics of participants who demonstrate enhancement in gait function with RAGT in this study. Conducting additional analysis of this aspect of the study would be highly significant. However, given that this analysis constitutes an interim analysis of the entire study, the investigation of factors such as cognitive function would be more appropriately conducted in a larger number of participants following the completion of the full study.
On conclusion, this study demonstrated that the overground gait training with a torque-assisted exoskeleton for four weeks represented a safe and efficacious method of gait rehabilitation in subacute stroke patients. Furthermore, the overground gait training with a torque-assisted exoskeleton could enhance gait function comparable to the conventional gait rehabilitation in subacute stroke patients, with additional gains in lower extremity strength. These findings suggest that the overground gait training with a torque-assisted exoskeleton might be a potential intervention for subacute stroke patients.

No comments:
Post a Comment