Since this was done at 12 months post stroke no survivor will be able to get this from an insurance paid therapist. Your insurance will have stopped because you plateaued out months prior. You're going to have to do this on your own. I'd suggest reading Margaret
Yekutiel who wrote a whole book about this in 2001, 'Sensory Re-Education
of the Hand After Stroke'? Not robotics, but doable.
Effects of a robot‐aided somatosensory training on proprioception and motor function in stroke survivors
Journal of NeuroEngineering and Rehabilitation volume 18, Article number: 77 (2021)
Abstract
Background
Proprioceptive deficits after stroke are associated with poor upper limb function, slower motor recovery, and decreased self-care ability. Improving proprioception should enhance motor control in stroke survivors, but current evidence is inconclusive. Thus, this study examined whether a robot-aided somatosensory-based training requiring increasingly accurate active wrist movements improves proprioceptive acuity as well as motor performance in chronic stroke.
Methods
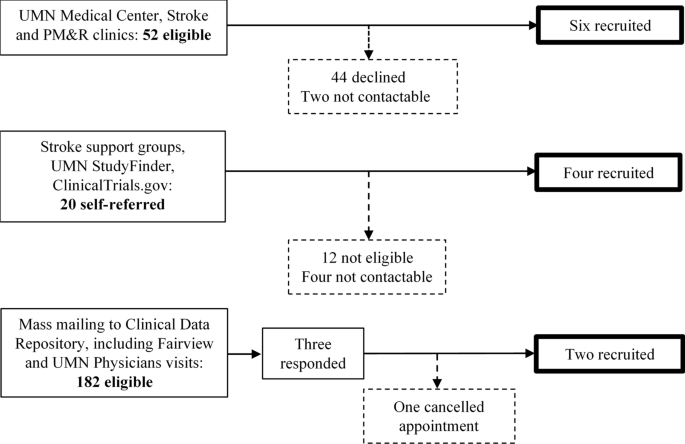
Twelve adults with chronic stroke completed a 2-day training (age range: 42–74 years; median time-after-stroke: 12 months; median Fugl–Meyer UE: 65). Retention was assessed at Day 5. Grasping the handle of a wrist-robotic exoskeleton, participants trained to roll a virtual ball to a target through continuous wrist adduction/abduction movements. During training vision was occluded, but participants received real-time, vibro-tactile feedback on their forearm about ball position and speed. Primary outcome was the just-noticeable-difference (JND) wrist position sense threshold as a measure of proprioceptive acuity. Secondary outcomes were spatial error in an untrained wrist tracing task and somatosensory-evoked potentials (SEP) as a neural correlate of proprioceptive function. Ten neurologically-intact adults were recruited to serve as non-stroke controls for matched age, gender and hand dominance (age range: 44 to 79 years; 6 women, 4 men).
Results
Participants significantly reduced JND thresholds at posttest and retention (Stroke group: pretest: mean: 1.77° [SD: 0.54°] to posttest mean: 1.38° [0.34°]; Control group: 1.50° [0.46°] to posttest mean: 1.45° [SD: 0.54°]; F[2,37] = 4.54, p = 0.017, ηp2 = 0.20) in both groups. A higher pretest JND threshold was associated with a higher threshold reduction at posttest and retention (r = − 0.86, − 0.90, p ≤ 0.001) among the stroke participants. Error in the untrained tracing task was reduced by 22 % at posttest, yielding an effect size of w = 0.13. Stroke participants exhibited significantly reduced P27-N30 peak-to-peak SEP amplitude at pretest (U = 11, p = 0.03) compared to the non-stroke group. SEP measures did not change systematically with training.
Conclusions
This study provides proof-of-concept that non-visual, proprioceptive training can induce fast, measurable improvements in proprioceptive function in chronic stroke survivors. There is encouraging but inconclusive evidence that such somatosensory learning transfers to untrained motor tasks.
Trial registration Clinicaltrials.gov; Registration ID: NCT02565407; Date of registration: 01/10/2015; URL: https://clinicaltrials.gov/ct2/show/NCT02565407.
Background
Nearly two-thirds of stroke survivors exhibit forms of somatosensory or proprioceptive dysfunction [1, 2]. Proprioceptive deficits are related to longer length-of-stay in hospitals [3], poor quality of movement, poorer activities of daily (ADL) function and reduced participation in physical activity [4,5,6]. Proprioceptive deficits predict treatment responses to robot-assisted motor retraining with augmented proprioceptive feedback [7] These may be explained by the crucial role of proprioception in motor control and learning [8, 9]. Proprioceptive training is a form of somatosensory intervention that aims to enhance proprioceptive function. Several forms of somatosensory intervention such as passive, repetitive cutaneous stimulation [10, 11], passive limb movement training [12], repeated somatosensory discrimination practice and active sensorimotor training with augmented somatosensory feedback [7, 13, 14, 15] have been proposed to aid recovery of proprioceptive function and motor function after stroke. Proprioceptive improvements observed after proprioceptive training interventions correlated with improvement of untrained motor performance in healthy young adults [16, 17]. This further supports the rationale to implement proprioceptive-motor training for people with stroke. Among all types of proprioceptive intervention, active sensorimotor training with augmented somatosensory feedback [7, 13,14,15] seem to produce consistent results across studies [1, 18]. These interventions often employ somatosensory signals either to replace visual feedback on motor performance or to augment existing visual and somatosensory feedback for online motor control. One well studied mode of somatosensory feedback is vibro-tactile feedback (VTF) applied to the skin surface. Incorporating VTF with movement training has been shown to improve the learning of simple motor tasks in healthy adults and clinical populations [19,20,21]. There is evidence that it can effectively enhance proprioceptive function [22].
Somatosensory evoked potentials (SEPs) recorded via electroencephalography (EEG) are an objective neurophysiological marker of somatosensory processing with established procedures and normative values that has been used among clinical populations. Adults after stroke typically present with a lower peak amplitude or longer peak latency of SEPs (e.g. [23, 24]). Moreover, the restoration of typical SEPs has been reported following somatosensory interventions [25, 26]. Thus, we here recorded SEP to verify changes in the neural processing of somatosensory signals in sensorimotor cortex as a function of the somatosensory-motor intervention employed in this project
.
To address if a somatosensory-based training is a meaningful approach for the rehabilitation of proprioceptive and motor function after stroke, this proof-of-concept study aimed to determine whether wrist proprioception could be trained in stroke survivors and whether such sensory learning transfers to other functional tasks involving the same joint and limb motor system.
No comments:
Post a Comment