What a novel idea, making rehab repeatable. Can you disseminate that to all stroke researchers?
Within- and between-therapist agreement on personalized parameters for robot-assisted gait therapy: the challenge of adjusting robotic assistance
Journal of NeuroEngineering and Rehabilitation volume 20, Article number: 81 (2023)
Abstract
Background
Stationary robotic gait trainers usually allow for adjustment of training parameters, including gait speed, body weight support and robotic assistance, to personalize therapy. Consequently, therapists personalize parameter settings to pursue a relevant therapy goal for each patient. Previous work has shown that the choice of parameters influences the behavior of patients. At the same time, randomized clinical trials usually do not report the applied settings and do not consider them in the interpretation of their results. The choice of adequate parameter settings therefore remains one of the major challenges that therapists face in everyday clinical practice. For therapy to be most effective, personalization should ideally result in repeatable parameter settings for repeatable therapy situations, irrespective of the therapist who adjusts the parameters. This has not yet been investigated. Therefore, the aim of the present study was to investigate the agreement of parameter settings from session to session within a therapist and between two different therapists in children and adolescents undergoing robot-assisted gait training.
Methods and results
Fourteen patients walked in the robotic gait trainer Lokomat on 2 days. Two therapists from a pool of 5 therapists independently personalized gait speed, bodyweight support and robotic assistance for a moderately and a vigorously intensive therapy task. There was a very high agreement within and between therapists for the parameters gait speed and bodyweight support, but a substantially lower agreement for robotic assistance.
Conclusion
These findings imply that therapists perform consistently at setting parameters that have a very clear and visible clinical effect (e.g. walking speed and bodyweight support). However, they have more difficulties with robotic assistance, which has a more ambiguous effect because patients may respond differently to changes. Future work should therefore focus on better understanding patient reactions to changes in robotic assistance and especially on how instructions can be employed to steer these reactions. To improve the agreement, we propose that therapists link their choice of robotic assistance to the individual therapy goals of the patients and closely guide the patients during walking with instructions.
Background
The improvement of walking functions is a major rehabilitation goal in neuropaediatric patients [1]. Rehabilitation research has established that goal-oriented therapy [2], lots of practice [3], and the patient’s active participation [4] are important contributors to a successful rehabilitation process. Therapists commonly use these motor learning principles to adapt therapy content to the needs of individual patients. However, scientific literature provides little evidence on the personalization of therapies. This can be partially attributed to the fact that describing therapy content in a rehabilitation context is challenging [5]. Whereas in the pharmaceutical context, therapy content can be clearly described by formulation, dose, and dosage, active rehabilitation interventions are not as clearly defined and can include a range of different activities/exercises/movements chosen by the therapist for specific patients. As a consequence, specific information about the therapy content is missing in many studies evaluating the effectiveness of physiotherapeutic interventions [6]. This applies also to modern robotic gait therapies [7, 8]. In the case of conventional therapies, reasons for the lack of information include missing tools which can quantify and describe the therapist-patient interactions. However, in modern robotic systems, control parameters set by the therapist and sensors measuring the patient's behavior allow for the quantification, storage, and study of information on therapist-patient interactions mediated by the device. Nevertheless, this information has been rarely used to better understand the therapist’s decision making process.
One example of such a platform is the widely used exoskeleton Lokomat (Hocoma AG, Volketswil, Switzerland [9]. The Lokomat provides the therapist with several parameters that can be tuned to challenge patients individually [10, 11]. The most commonly used parameters are the regulation of gait speed, the amount of unloading via a harness called the bodyweight support, and a scaling factor for the force field, that keeps the hip and knee joints on the desired angular trajectory, called the Guidance Force [12]. In addition, the robotic assistance can also be tuned with a newer control mode named Path Control to allow for temporal variability [11]. It is known from research focusing on the device-patient interaction that all these parameter settings can influence patient behavior [11, 13, 14]. The desired physiologic reaction, which depends on the therapy goal, may vary between patients due to factors such as the day's condition, the underlying disease, motivation, or the relationship with the therapist. Therefore, the optimization of parameter settings cannot be performed with a single objective function for all patients, but different objectives must be carefully selected and weighted. Consequently, finding optimal parameter settings remains an important task in the responsibility of the therapist. That therapists perform well at this task is a key assumption of many clinical studies [15,16,17,18,19]. A consistent strategy is critical to ensure the validity and repeatability of this type of therapy in clinical practice and a prerequisite for the generalizability of clinical studies results. To the best of our knowledge, no study has investigated the agreement of the choice of parameter settings between and within therapists.
Therefore, the aim of the present study was to investigate the agreement on Lokomat parameter settings from session to session within a therapist and between two different therapists in a pediatric population. To this end, we developed a cross-sectional study protocol asking therapists to individualize therapy parameters for two therapy situations mimicking a real world therapy scenario. Our hypothesis was that the chosen parameter settings agree well within a single therapist and between therapists who received a similar training, with a higher agreement within therapists than between therapists.
Methods
Ethical approval for the study was obtained from the Cantonal Ethics Committee Zurich (BASEC Nr. 21-D0044), and the study procedures were in accordance with the Declaration of Helsinki.
Participants
Children and adolescents with a neurologic gait disorder were recruited by convenience sampling between November 2021 and March 2022. Patients between 5 and 18 years old were included. Exclusion criteria were the presence of any factor that prevented the usage of the Lokomat as specified in the device’s handbook [20]. Patients were also excluded if they were unable to follow the study instructions or to communicate pain and discomfort. Written informed consent was provided by the legal guardian of each participant and by the participants themselves if they were 12 years or older.
Study procedures
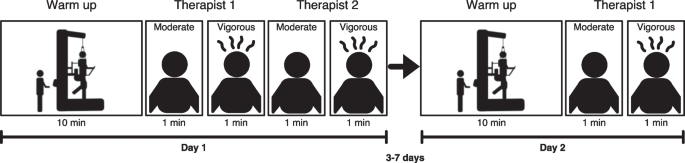
The study participants were asked to walk with the LokomatPro Version 6 (Hocoma, Volketswil, Switzerland) on two days. Each of the visits contained about 20 min. of actual walking time. During the first 10 min., patients could accommodate themselves to the device. Two different comparisons were performed: (1) Between-therapist agreement was assessed on the first day by asking two therapists to independently set Lokomat parameters (see Fig. 1). Within-therapist agreement was assessed by asking the first therapist to re-set the parameters at a second visit 3–7 days apart (see Fig. 1). During the parameter setting, therapists were blinded to previously selected parameters by themselves and their peer. The duration of 3–7 days was chosen as a trade-off between a possible memorization of the parameter settings by the therapist and training effects of the patient that could influence the results.
Study design: participants walked for 10 min. in the Lokomat to accommodate themselves. Then, therapists were asked to personalize the device parameters to two target intensities by choosing an appropriate combination of gait speed, bodyweight support, and robotic assistance. After the therapists confirmed their choice, participants walked for 1 min. with the selected parameters. The parameters selected by Therapist 1 and Therapist 2 on Day 1 were used to calculate between-therapist agreement. 3–7 days after the first visit Therapist 1 repeated the task to evaluate within-therapist agreement
Pairs from the five therapists from the robotics team at the Swiss Children’s Rehab were involved in the study procedures. Thus, 10 different combinations of pairings were possible. All therapists received a similar training and were experienced in Lokomat therapy. The education concept at the Swiss Children’s Rehab includes 5 sessions of one on one training on the device with a test person without impairments, followed by a minimum of 10 sessions of supervised therapies. The first three months include at least 4 therapies per day and a regular exchange with supervisors. Supervisors are therapists with several years of experience and an additional education in gait analysis. The therapy team meets every 2–4 weeks to discuss new literature and therapy approaches.
For the present study, comparable test conditions were created, that mimic real-world therapy situations, by giving therapists a defined therapy goal (“reproduce a physiological gait pattern”) and two different target intensities. They were instructed to set the Lokomat parameters as follows: The target intensity of the first condition was “Moderate”, such that the patient would be able to walk for 30 min. while maintaining a physiological gait pattern. The target intensity of the second condition was “Vigorous”, such that the patient would be able to maintain a physiologic gait pattern for a maximum of 5 min. These two conditions allow to investigate both, baseline parameter settings as well as parameter settings with which therapists try to repeatedly challenge patients for short periods.
The therapists could modify three parameters in this study, namely gait speed, bodyweight support, and the robotic assistance (Table 1). Robotic assistance in the Lokomat consists of two superposing components, namely Guidance Force and Path Control, whereby Path Control is only enabled below 50% Guidance Force. To obtain a single value for robotic assistance, therapists were instructed to work with Guidance Force until 40% and then switch to Path Control to further decrease robotic assistance. To quantify total robotic assistance in this study, Guidance Force and Path Control were added to a single compound parameter of robotic assistance ranging from 200 to 40%. Values between 200 and 140% were achieved by adjusting Guidance Force and values from than 140 to 40% by adjusting Path Control. As an example, if a therapist chooses a Guidance Force level of 40% and a Path Control level of 70%, this would result in a robotic assistance of 110% (40% + 70%). Once the therapists confirmed their choice, the patients walked for one minute with the selected parameters. This phase ensured that the parameters were feasible, especially in the vigorous condition, and that participants could actually walk without stumbling or safety stops. If necessary, therapists were allowed to instruct the patients with a set of standardized sentences (Additional file 1). The final parameters were noted down for analysis.
Data analysis
All statistical analyses were performed in RStudio (RStudio Team, 2015. RStudio: Integrated Development for R. RStudio, Inc., Boston, MA, USA). The within-therapist and between-therapist agreement was evaluated as follows: For each parameter and condition, thresholds that cover 50%, 75% and 100% of the absolute differences were calculated. In addition, Bland–Altman statistics were performed to estimate the agreement by the Limits of Agreement [21]. To evaluate whether the moderate and vigorous condition resulted in different parameter settings, the mean difference over all patients was calculated. The moderate and vigorous conditions were tested for statistical difference with paired t-tests and we applied a Bonferroni correction for multiple comparisons.
Results
Of the 14 participants, that were included, 11 completed all conditions. For two participants, only one therapist was available due to sickness of therapists or holidays. One patient could not complete the second visit because of wounds at the feet. Therefore, 13 participants were included in the within-therapist analysis and 12 participants were included in the between-therapist analysis. Detailed information about the patients can be found in Additional file 2.
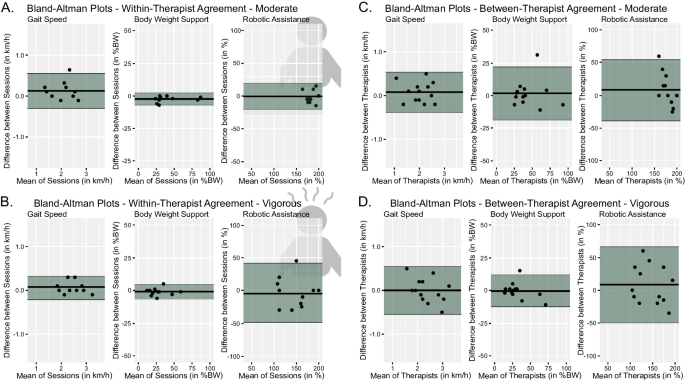
Within-therapist agreement
The difference within the same therapist in gait speed was less than 0.2 km/h for the moderate condition and 0.1 km/h for the vigorous condition in at least 75% of the participants (Table 2). Similarly, the difference in bodyweight support was less than 4% of the bodyweight for both conditions (Table 2). The agreement in robotic assistance was lower, especially for the vigorous condition where the difference was bigger than 28% in half of the participants (Table 2). In general, the agreement was high within the same therapist (Fig. 2A, B).
Illustrates the Bland–Altman Plots for the differences of the three parameters per condition. The black lines indicates the mean difference while the green areas mark the Limits of Agreement. A, B show the within-therapist agreement. C, D show the between-therapist agreement. The spread of the selected parameters can be seen on the respective x-axis. BW bodyweight
Between-therapist agreement
For between-therapist agreement, differences in gait speed settings were similar to the within-therapist differences (Table 2). The differences in bodyweight support were slightly larger between therapists than within therapists (Table 2). Robotic assistance differed more than 25% between therapists in half of the participants but, in contrast to the within-therapist differences, this was the case in both the moderate and the vigorous condition.
The Bland–Altman statistics revealed a relatively even distribution with mean values close to 0. The exception were robotic assistance settings where the difference between therapists was slightly skewed. The distribution of the individual differences is presented in Fig. 2.
The parameter settings for the moderate and the vigorous condition differed significantly for all three parameters. Participants walked significantly faster with lower bodyweight support and lower robotic assistance during the vigorous condition (Table 3).
Discussion
We found a high agreement for gait speed and bodyweight support settings as indicated by the small absolute differences. This means that therapists select very comparable gait speed and bodyweight support settings for the same patient in two consecutive trainings when given a similar training goal. This agreement was lower for robotic assistance. In general, the within-therapist agreement was slightly higher than the between-therapist agreement. These findings hold true for both therapy conditions, despite the statistically significant differences in parameter settings between the two conditions.
No comments:
Post a Comment