WHOM from your hospital is assigned to follow this research and get it implemented if successful? If you don't have such a person, you don't have a functioning stroke hospital.
ELECTRA-STROKE: Electroencephalography controlled triage in the ambulance for acute ischemic stroke—Study protocol for a diagnostic trial
- 1Department of Clinical Neurophysiology, Amsterdam University Medical Centers (UMC) Location University of Amsterdam, Amsterdam, Netherlands
- 2Department of Neurology, Amsterdam UMC Location University of Amsterdam, Amsterdam, Netherlands
- 3Witte Kruis Ambulancezorg, Alkmaar, Netherlands
- 4Ambulancezorg Nederland, Zwolle, Netherlands
- 5Ambulance Amsterdam, Amsterdam, Netherlands
- 6Department of Biomedical Engineering and Physics, Amsterdam UMC Location University of Amsterdam, Amsterdam, Netherlands
- 7Department of Radiology and Nuclear Medicine, Amsterdam UMC Location University of Amsterdam, Amsterdam, Netherlands
Background: Endovascular thrombectomy (EVT) is the standard treatment for large vessel occlusion stroke of the anterior circulation (LVO-a stroke). Approximately half of EVT-eligible patients are initially presented to hospitals that do not offer EVT. Subsequent inter-hospital transfer delays treatment, which negatively affects patients' prognosis. Prehospital identification of patients with LVO-a stroke would allow direct transportation of these patients to an EVT-capable center. Electroencephalography (EEG) may be suitable for this purpose because of its sensitivity to cerebral ischemia. The hypothesis of ELECTRA-STROKE is that dry electrode EEG is feasible for prehospital detection of LVO-a stroke.
Methods: ELECTRA-STROKE is an investigator-initiated, diagnostic study. EEG recordings will be performed in patients with a suspected stroke in the ambulance. The primary endpoint is the diagnostic accuracy of the theta/alpha ratio for the diagnosis of LVO-a stroke, expressed by the area under the receiver operating characteristic (ROC) curve. EEG recordings will be performed in 386 patients.
Discussion: If EEG can be used to identify LVO-a stroke patients with sufficiently high diagnostic accuracy, it may enable direct routing of these patients to an EVT-capable center, thereby reducing time-to-treatment and improving patient outcomes.
Clinical trial registration: ClinicalTrials.gov, identifier: NCT03699397.
Introduction
Stroke is the world's second leading cause of death and the third leading cause of death and disability combined (1). For more than two decades, intravenous thrombolysis (IVT) has been the standard treatment for acute ischemic stroke (AIS) (2). In 2015, various randomized controlled trials established the efficacy of endovascular thrombectomy (EVT) in patients with large vessel occlusion stroke of the anterior circulation (LVO-a stroke) (3), and EVT has since become standard therapy for this population (4, 5). For both IVT and EVT, early initiation of treatment is of the utmost importance, as patient outcome reduces with increasing time-to-treatment (6).
While IVT is available in most hospitals, EVT is—because of its complexity and required resources—only performed in selected hospitals, so-called comprehensive stroke centers (CSCs). Currently, ~45–55% of EVT-eligible patients are initially referred to primary stroke centers (PSCs), which are hospitals that do not provide this therapy (7–9). After initial workup, patients with LVO-a stroke must be transferred to a CSC. This workflow substantially delays the initiation of EVT, which has a negative effect on patient outcomes (6, 10). A study in the Netherlands found that the initial presentation of patients with LVO-a stroke in a PSC resulted in a delay of EVT by 1 h on average which was associated with an absolute decrease in the chance of functional independence at 3 months by 8.5% (7, 11). In other countries, the delay of EVT varied between 40 and 115 min in patients transferred to a CSC when compared with patients who were directly presented to a CSC (9, 12–14).
Since only a small proportion, ~12%, of all patients with a suspected stroke is eligible for EVT (15), it is not feasible to transport all patients with suspected stroke directly to a CSC. This would not only challenge the capacity of ambulance services and CSCs, but it would also lead to an unnecessary delay in the initiation of therapy in patients who require IVT but not EVT, as these patients would be subjected to a longer travel time.
A triage method that reliably identifies patients with LVO-a stroke in the ambulance would allow for patients with LVO-a stroke to be directly transported to a CSC, while patients without LVO-a stroke could still be transported to the nearest PSC (Figure 1). Several triage methods have been proposed for this purpose, but none of these methods are currently considered suitable for broad implementation (16). For example, multiple studies on the use of Mobile Stroke Units for prehospital diagnosis and treatment of acute ischemic stroke have been conducted. These studies show a positive effect of Mobile Stroke Units on the functional outcomes of patients (17–19). However, the costs of Mobile Stroke Units are high (20, 21), which makes broad implementation difficult.
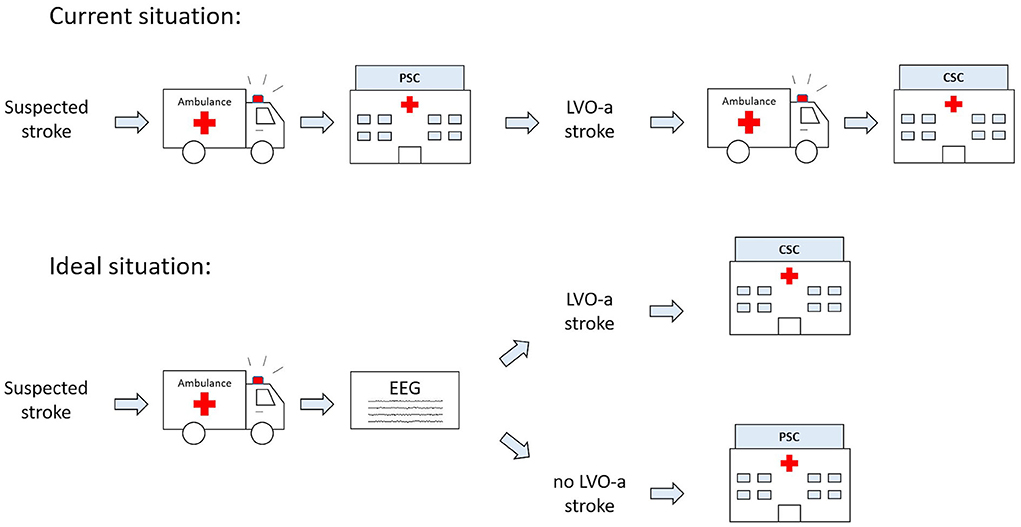
Figure 1. Current and future ideal prehospital workflow for patients with suspected acute ischemic stroke (AIS). CSC, comprehensive stroke center; EEG, electroencephalography; LVO-a, large vessel occlusion of the anterior circulation; PSC, primary stroke center.
Electroencephalography (EEG) may be suitable as a prehospital triage method since EEG is highly sensitive to changes in neuronal function caused by brain ischemia (22). Previous studies have shown that a decrease in cerebral blood flow results in a slowing of the EEG signal within seconds (23, 24). Multiple case-control studies have found that ratios between slow and fast EEG activity, such as the delta/alpha ratio, discriminate between patients with AIS and healthy controls (25, 26). Few studies have been conducted on the use of EEG to identify LVO stroke in patients with suspected acute ischemic stroke (27, 28). A study used a portable LVO detection device using EEG and somatosensory-evoked potentials and demonstrated high LVO discrimination (C-statistic: 0.88) (29). Another study used a dry electrode EEG system and reported a high diagnostic accuracy for LVO stroke detection when combining clinical and EEG data [area under the receiver operating characteristic (ROC) curve: 87.8] (30). All these studies, however, were conducted in the emergency room and not in the prehospital setting.
We hypothesize that EEG accurately identifies the presence of an LVO-a stroke in patients with a suspected stroke when applied in the ambulance. The aim of the ELECTRA-STROKE study is to determine the diagnostic accuracy of dry electrode cap EEG for the diagnosis of LVO-a stroke when performed by ambulance personnel in patients with a suspected stroke.
More at link.
 Maritta N. van Stigt
Maritta N. van Stigt Anita A. G. A. van de Munckhof
Anita A. G. A. van de Munckhof Laura C. C. van Meenen
Laura C. C. van Meenen Eva A. Groenendijk1,2,
Eva A. Groenendijk1,2,  Henk A. Marquering
Henk A. Marquering Charles B. L. M. Majoie
Charles B. L. M. Majoie Yvo B. W. E. M. Roos
Yvo B. W. E. M. Roos Johannes H. T. M. Koelman
Johannes H. T. M. Koelman Wouter V. Potters
Wouter V. Potters Jonathan M. Coutinho
Jonathan M. Coutinho
No comments:
Post a Comment