She may be certified and much more professionally trained than me but still has NO protocol written up on this. Survivors demand better!
National Stroke Awareness Month: Vagus Nerve Stimulation Post-Stroke
Written By: Liza Meiksins PT, DPT
Board Certified Specialist in Neurologic Physical Therapy
Certified Lymphedema Therapist
Many patients and therapists would likely agree that one of the most challenging aspects of stroke rehab is improving upper extremity function and recovery. As a former patient once said, “I would be happy with my recovery if this arm just wasn’t so stubborn!” But with few options to promote upper extremity recovery, there has been a lot of talk recently about the use of vagus nerve stimulation. So, what exactly is vagus nerve stimulation and how does it impact upper extremity recovery post-stroke?
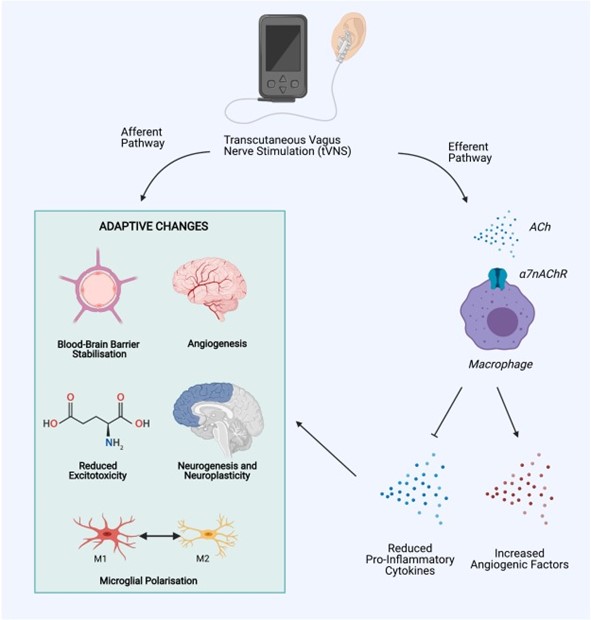
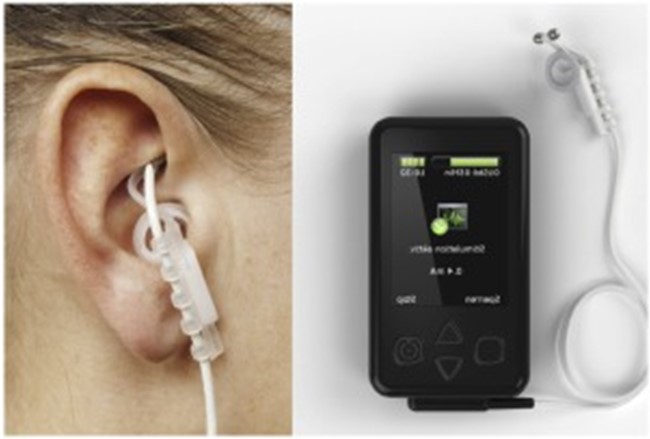
Invasive vagus nerve stimulation (i-VNS) has been widely accepted to improve upper extremity function post-stroke, but this requires a surgical procedure and is not appropriate nor encouraged for many patients1. However, in recent years, transcutaneous vagus nerve stimulation (t-VNS) has been shown to activate similar vagal nerve projections as i-VNS and is generally safe and well-tolerated1. t-VNS can be carried out through auricular VNS in the ear or cervical branch VNS in the neck and has been shown to elicit the following responses:
Physiologic Changes with t-VNS1,2:
- Cholinergic & monoaminergic modulation of motor cortex neurons
- Reduced systemic inflammation
- Reduced blood-brain barrier breakdown
- Increased angiogenesis
- Reduced excitotoxicity
- Improved axon regeneration & reorganization
Functional Outcomes with t-VNS1,2,3:
- Significant improvement in immediate and long-term upper extremity outcomes when t-VNS was applied in conjunction with intensive, task-specific rehabilitation (quantified using the UE Fugl-Meyer scale, Wolf Motor Function Test, Stroke Impact Scale, and Motor Activity Log)
- Most research has been done on patients with moderate-severe UE impairment
- Results consistent in both sub-acute and chronic strokes
- Most studies have examined the use of t-VNS immediately prior to rehab interventions and used auricular VNS as the method of delivery
Further research(EXACTLY WHOM is doing that? So we can follow up and make sure it gets done.) continues to be carried out to expand our understanding of dosing, optimal patient selection, laterality, and auricular vs cervical stimulation, among other variables to optimize outcomes. There is also the potential to utilize t-VNS for other impairments besides motor function, including: dysphagia, dysphasia, cognition, and visual field dysfunction1.
While many questions surrounding transcutaneous vagus nerve stimulation still abound, it remains an extremely promising intervention to potentiate rehabilitation-driven neuroplasticity and improve functional outcomes for our patients post-stroke!
Explore online continuing education courses from Liza below:
Clinical Application of Neuromuscular Electrical Stimulation (NMES) for Neurologic Conditions
High-Intensity Gait Training for Stroke and Spinal Cord Injury Patients
Visit summit-education.com for more information.
References:
Baig SS, Kamarova M, Ali A et al. Transcutaneous vagus nerve stimulation (tVNS) in stroke: the evidence, challenges and future directions. J Autonom Neurosci. 2022;237.
Dawson J, Liu CY, Francisco GE, et al. Vagus nerve stimulation paired with rehabilitation for upper limb motor function after ischaemic stroke (VNS-REHAB): a randomised, blinded, pivotal, device trial. The Lancet. 2021;397(10284):1545-1553.
Hamer HM, Bauer S. Lessons learned from transcutaneous vagus nerve stimulation (tVNS). Epilepsy Research. 2019;153:83-84.
Lui Y, Zhang L, Zhang X, et al. Effect of Combined Vagus Nerve Stimulation on Recovery of Upper Extremity Function in Patients with Stroke: A Systematic Review and Meta-Analysis. J Stroke Cerebrovas Dis. 2022;31(6)
No comments:
Post a Comment