Evaluations DO NOTHING FOR RECOVERY! Survivors would like exact recovery protocols. GET THERE! I'd fire you all.
Novel evaluation of upper-limb motor performance after stroke based on normal reaching movement model
Journal of NeuroEngineering and Rehabilitation volume 20, Article number: 66 (2023)
Abstract
Background
Upper-limb rehabilitation robots provide repetitive reaching movement training to post-stroke patients. Beyond a pre-determined set of movements, a robot-aided training protocol requires optimization to account for the individuals’ unique motor characteristics. Therefore, an objective evaluation method should consider the pre-stroke motor performance of the affected arm to compare one’s performance relative to normalcy. However, no study has attempted to evaluate performance based on an individual’s normal performance. Herein, we present a novel method for evaluating upper limb motor performance after a stroke based on a normal reaching movement model.
Methods
To represent the normal reaching performance of individuals, we opted for three candidate models: (1) Fitts’ law for the speed-accuracy relationship, (2) the Almanji model for the mouse-pointing task of cerebral palsy, and (3) our proposed model. We first obtained the kinematic data of healthy (n = 12) and post-stroke (n = 7) subjects with a robot to validate the model and evaluation method and conducted a pilot study with a group of post-stroke patients (n = 12) in a clinical setting. Using the models obtained from the reaching performance of the less-affected arm, we predicted the patients’ normal reaching performance to set the standard for evaluating the affected arm.
Results
We verified that the proposed normal reaching model identifies the reaching of all healthy (n = 12) and less-affected arm (n = 19; 16 of them showed an R2 > 0.7) but did not identify erroneous reaching of the affected arm. Furthermore, our evaluation method intuitively and visually demonstrated the unique motor characteristics of the affected arms.
Conclusions
The proposed method can be used to evaluate an individual’s reaching characteristics based on an individuals normal reaching model. It has the potential to provide individualized training by prioritizing a set of reaching movements.
Background
Reaching movement (RM), among the most important recovery goals of stroke rehabilitation, represents inter-joint coordination in activities of daily living [1]. Rehabilitation robots can provide repetitive reaching training to post-stroke patients, whereas conventional rehabilitation modalities are labor intensive [2,3,4]. Beyond a predetermined and fixed set of movements, the training protocol will be more effective when optimized based on patient-specific needs for motor recovery [5,6,7]. Hence, the individualization of robotic therapy is required to account for an individual’s unique motor characteristics, resulting in varying motor performance and learning capacities [8, 9]. Therefore, an evaluation method that can objectively identify a patient’s motor characteristics is required for individualized robot-aided reaching training.
A well-established rehabilitation process entails the evaluation of the progress and effect of robotic intervention on an individual’s rehabilitation goals [10, 11]. Because the process would be directing an impaired task to progress toward a normal task [12,13,14], the evaluation of the RM needs to address the level of motor impairment of the affected limb based on the individual’s pre-stroke motor capacity, to demonstrate one’s reaching performance level relative to normalcy. Particularly, it is well known that understanding one’s desired recovery is a significant biomarker for prescribing the rehabilitation dose [15]. Hence, normal reaching characteristic information, which varies across individuals [8], needs to be the standard that sets a basis for the patients’ current reaching performance.
Several studies have utilized evaluation methods based on kinematic characteristics for the upper-limb motor ability and function in post-stroke patients during robot-aided therapy [9, 16,17,18,19,20] and have characterized the relative motor deficits of the affected limb in various directions or distances. However, they did not evaluate motor characteristics based on an individual’s normal performance; thus, the training effect was relatively evaluated before and after treatment, which does not consider the individual’s rehabilitation goal [9, 16,17,18,19,20]. In contrast, evaluating a patient’s current performance based on their normal performance provides an individually scaled motor deficit, which results in an objective evaluation of the robot-aided therapeutic effect. Therefore, it is necessary to understand the normal (original) reaching performance before stroke onset in a patient-specific manner to enhance the evaluations of individualized robotic reaching training.
However, it is unfeasible for patients to possess knowledge or data on their quantified normal reaching performance. Thus, an estimation method that can identify the before-onset reaching abilities of individuals is required. A plausible approach for estimating the patients’ normal reaching performance is to model the performance based on their less-affected arm; however, to the best of our knowledge, no such attempt has been made to date. Based on several studies that reported the similarity in motor performance between the post-stroke patients’ less-affected arms and healthy individuals’ arms [21,22,23], we posit that this approach could represent the normal reaching ability of post-stroke individuals. Here, the model needs to (1) represent one’s normal reaching ability well, and (2) not characterize one’s erroneous RM. Such a model can take task information (i.e., target distance) and human kinematic information (i.e., movement speed) as inputs and predict the movement time of the normal RM as an output.
Despite the above approach, the issue of how to model the less-affected arm persists. Several statistical models have captured quantifiable reaching characteristics [24,25,26]; however, to the best of our knowledge, there is no appropriate model for evaluating the normal RM of stroke. Fitts’ law, which is the most well-known reaching model [24], has been applied to quantify the reaching performance of stroke survivors. Although this method was simple and feasible for motor recovery, the results showed model inaccuracy under Fitts’ law [27]. This poor accuracy of Fitts’ law was also indicated by another study that modeled the reaching-related movements of patients with cerebral palsy (CP) [26]. To improve accuracy, a novel model that showed good accuracy was developed for CP movements [26]. However, the model was too complex and was not validated by the RM of stroke survivors.
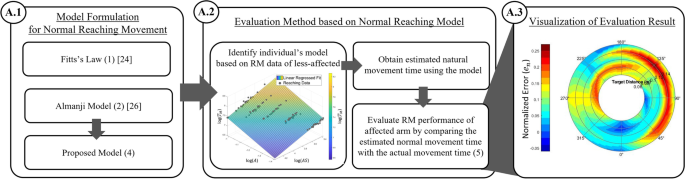
This study developed a novel evaluation method for individualized reaching training. We first identified a novel normal reaching model and formulated a method for evaluating motor deficits based on the proposed model of the less-affected arm. We then utilized the evaluated metrics to express an individual’s motor deficit as a contour map of the workspace [19, 20]. To validate the results, statistical analyses were conducted using experimental RM data collected from 12 healthy subjects and 19 patients with stroke. The results showed that the proposed method could enable individually scaled RM evaluation by comparing the performance of the affected arm with that of the normal reaching model of the less-affected arm.
Methods
Individually scaled evaluation method
In this subsection, we present candidate reaching models for describing the normal RM and explain how we derived the normal reaching model for post-stroke patients. Subsequently, based on the model, we defined the individually scaled performance index and visually mapped it for the evaluation method (Fig. 1).
Development process of individually scaled evaluation method. The blocks of the development procedures are denoted with marked circles in the following sections in Methods. Once an appropriate model for a normal RM is established, A.2 and A.3 are the general steps for utilizing the proposed evaluation method
No comments:
Post a Comment