For me body weight supported treadmill training was worthless. I needed the weight of my body to counteract the spasticity of my legs. And since spasticity never goes away, even now as I'm chronic this would do no good. Overground training is much better in my opinion since it normally gives you perturbations you need to deal with, giving you better balance and preventing falls.
Effects of dynamic body weight support on functional independence measures in acute ischemic stroke: a retrospective cohort study
Journal of NeuroEngineering and Rehabilitation volume 20, Article number: 6 (2023)
Abstract
Background
Stroke remains a major public health concern in the United States and a leading cause of long-term disability in adults. Dynamic body weight support (DBWS) systems are popular technology available for use in clinical settings such inpatient rehabilitation. However, there remains limited studies in such inpatient settings that compare DBWS to standard of care (SOC) using real world outcome measures. For survivors of acute ischemic stroke, we determine if incorporating a dynamic body weight support (DBWS) system into inpatient therapy offers greater improvement than standard of care (SOC).
Methods
A retrospective chart review included 52 individuals with an acute ischemic stroke admitted to an inpatient rehabilitation facility. Functional Independence Measure (FIM) data, specifically changes in FIM at discharge, served as the primary outcome measure. Patient cohorts received either therapies per SOC or therapies incorporating DBWS. Regardless of cohort group, all patients underwent therapies for 3 h per day for 5 days a week.
Results
For both groups, a statistically and clinically significant increase in total FIM (P < 0.0001) was observed at discharge compared to at admission. Improvements for the DBWS group were significantly greater than the SOC group as evidenced by higher gains in total FIM (p = 0.04) and this corresponded to a medium effect size (Cohen’s d = 0.58). Among FIM subscores, the DBWS group achieved a significant increase in sphincter control while all other subscore changes remained non-significant.
Conclusions
This preliminary evidence supports the benefit of using DBWS during inpatient rehabilitation in individuals who have experienced an acute ischemic stroke. This may be due to the greater intensity and repetitions of tasks allowed by DBWS. These preliminary findings warrant further investigations on the use of DBWS in inpatient settings.
Introduction
Stroke continues to be a major public health concern in the United States and one of the leading causes of long-term disability in adults with approximately 795,000 new cases every year [1]. Unfortunately, as evidenced by ischemic stroke incidence and stroke mortality, the stroke burden is unfortunately increasing in some regions of the country and particularly areas with socioeconomic and healthcare disparities [2, 3]. While significant advancement in recent medical care has increased survival post-stroke, approximately 5 million Americans are still living with residual deficits with an estimated healthcare cost of $46 billion each year. Stroke-related healthcare costs are projected to reach more than $94 billion per year by 2035 in the United States [1]. Therefore, it is of paramount importance to find new ways to improve rehabilitation outcomes and quality of life for people with stroke.
The concept of neuroplasticity plays a crucial role in rehabilitation outcomes [4]. Remarkable neuroplastic changes in corticospinal systems have been demonstrated during and/or after the intense performance of motor activities [5]. Generally speaking, neuroplastic change occurs more readily as activities become more intensive and repetitive with progressive challenges and salience [6]. Such activities have a greater likelihood of leading to lasting change in functional performance if the activities require active participation, problem-solving, and attention to task. It has also been known for a while now that the potential for functional recovery after stroke is greatest during the first 3–6 months following a stroke [7, 8]. Therefore, inpatient rehabilitation occurs during a pivotal time frame from a neuroplasticity perspective.
However, for patients with considerable motor and balance impairments, it is very difficult even in an inpatient setting to implement therapy repetitions with the aforementioned intensity, salience, and progressive challenge [9]. These patients have a justified fear of falling. Moreover, the fall risk is difficult to manage solely with therapy personnel as the current rehabilitation setting in the United States features an already high patient-therapist ratio [10]. Conceivably, the fall risk and the fear of falling are detrimental for neuroplasticity: (a) the attention of the patient and therapist can be more focused on safety measures and distracted from the motor task itself; (b) therapists may select tasks that are safer in lieu of challenging tasks that are more conducive to neuroplastic changes; and (c) repetition goals may be too conservative due to concerns of patient fatigue and the increased fall risk associated with fatigue [11]. These conservative repetition goals in current standards of care are evidenced by a recent study reporting very limited daily step counts for patients undergoing inpatient stroke rehabilitation [12].
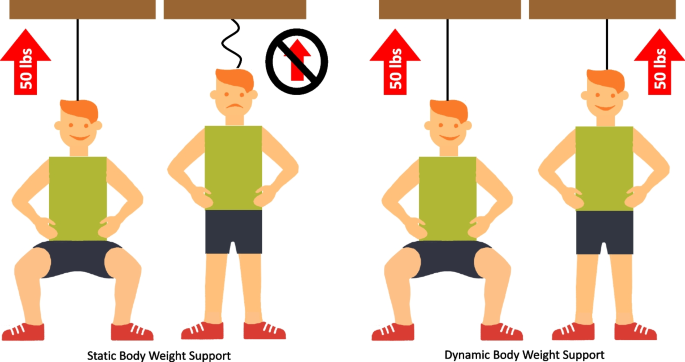
Dynamic body weight support (DBWS) systems are a popular set of technologies that facilitate over-ground therapy and are designed to unload body weight more consistently during dynamic conditions such as movement-based therapy (Fig. 1). This consistent unloading is achieved by means of a sensor, an actuator, and an onboard computer controller. The controller is crucial to creating a feedback control loop, which constantly compares measured load versus the desired load and adjusts rope tension accordingly by means of the actuator. The onboard computer controller inherent to these systems allows novel safety features to reduce fall risk—automatic fall detection and an injury prevention mode. In addition, these systems allow real-time feedback for participants owing to the visual displays of real-time sensor data. By facilitating safe therapy and real-time feedback, DBWS has the potential to foster principles of neuroplasticity. That is, participants may better focus their attention and they may be more motivated for therapeutic activities. Our group has reported beneficial effects of DBWS on inpatient discharge outcomes compared to standard of care in patient populations such as traumatic brain injury and spinal cord injuries [13, 14]. However, it is not known if DBWS can also lead to greater functional recovery during inpatient rehabilitation in a population with an acute ischemic stroke, which is the motivation for this study. In the present study, we evaluate whether over-ground gait and balance training incorporating DBWS leads to greater functional recovery after an acute ischemic stroke compared to standard of care (SOC) as assessed by the Functional Independence Measure (FIM).
No comments:
Post a Comment