I see nothing here that even remotely suggests that an objective damage diagnosis was done to set a baseline for making this research repeatable. So bad research.
Effects of a soft robotic exosuit on the quality and speed of overground walking depends on walking ability after stroke
Journal of NeuroEngineering and Rehabilitation volume 20, Article number: 113 (2023)
Abstract
Background
Soft robotic exosuits can provide partial dorsiflexor and plantarflexor support in parallel with paretic muscles to improve poststroke walking capacity. Previous results indicate that baseline walking ability may impact a user’s ability to leverage the exosuit assistance, while the effects on continuous walking, walking stability, and muscle slacking have not been evaluated. Here we evaluated the effects of a portable ankle exosuit during continuous comfortable overground walking in 19 individuals with chronic hemiparesis. We also compared two speed-based subgroups (threshold: 0.93 m/s) to address poststroke heterogeneity.
Methods
We refined a previously developed portable lightweight soft exosuit to support continuous overground walking. We compared five minutes of continuous walking in a laboratory with the exosuit to walking without the exosuit in terms of ground clearance, foot landing and propulsion, as well as the energy cost of transport, walking stability and plantarflexor muscle slacking.
Results
Exosuit assistance was associated with improvements in the targeted gait impairments: 22% increase in ground clearance during swing, 5° increase in foot-to-floor angle at initial contact, and 22% increase in the center-of-mass propulsion during push-off. The improvements in propulsion and foot landing contributed to a 6.7% (0.04 m/s) increase in walking speed (R2 = 0.82). This enhancement in gait function was achieved without deterioration in muscle effort, stability or cost of transport. Subgroup analyses revealed that all individuals profited from ground clearance support, but slower individuals leveraged plantarflexor assistance to improve propulsion by 35% to walk 13% faster, while faster individuals did not change either.
Conclusions
The immediate restorative benefits of the exosuit presented here underline its promise for rehabilitative gait training in poststroke individuals.
Background
Stroke is a leading cause of serious long-term disability that results in a slow, unstable, and energetically inefficient gait. Paresis of the muscles on one side of the body contributes to asymmetric walking patterns poststroke. Impaired plantarflexor muscle activity on the paretic side results in reduced propulsive force [1], whereas impaired dorsiflexor activity results in reduced ground clearance and impaired limb loading [2,3,4,5]. Together, these impairments increase the risk of falling, which is often compensated for by hip hiking and hip circumduction strategies [6, 7]. These mobility deficits can hinder social participation and affect the quality of life [8], warranting the development of interventions that restore paretic plantarflexor and dorsiflexor function during walking [9].
For people with neurological conditions, wearable robots have the potential to help restore mobility. Rigid exoskeletons that provide full body weight and limb advancement support have been shown to be beneficial for non-ambulatory individuals with for instance a complete spinal cord injury [10, 11], but mixed results are found for ambulatory individuals with gait impairments such as most stroke survivors [10,11,12,13]. In fact, the high levels of assistance might reduce the user’s neuromuscular activity [14,15,16]. Because active engagement is crucial for the experience-dependent plasticity that underlies motor recovery, the partial support provided by soft robotic exosuits are a promising therapeutic alternative to keep neuromuscular slacking to a minimum.
We developed a soft robotic exosuit to provide paretic plantarflexor assistance to enhance propulsion during the push-off phase and paretic dorsiflexor assistance to improve ground clearance during the swing phase and foot landing during the loading phase [17, 18]. This lightweight wearable device applies assistance via Bowden cables that connect to garment-like, functional textile anchors on the shank and foot. The textile-based interface allows exosuits to operate in parallel with the user’s paretic muscles to augment, not replace, their movements. Our previous studies with a tethered exosuit and a preliminary version of the portable exosuit (5 kg total weight including motors and batteries worn at the waist) reported improvements in the mechanics, energetics, and functional walking capacity of a small cohort of community-dwelling people poststroke compared to walking with an exosuit unpowered [17, 19, 20] or walking without an exosuit [19, 21,22,23].
Motivated by these findings, we refined the form factor, usability, comfort, power consumption as well as the paretic gait event detection and cable position control algorithms of the portable exosuit, reducing its weight by nearly 25% to 3.8 kg (see Methods) [20]. The updated portable exosuit (Fig. 1) is designed to support long-distance overground walking, similar to everyday walking. Therefore, the purpose of this study is to extend our preliminary findings to a larger sample of individuals with chronic (> 6 months) poststroke hemiparesis by evaluating the immediate effects of plantarflexor and dorsiflexor assistance during continuous overground walking in the laboratory at a comfortable walking speed, compared to walking without an exosuit.
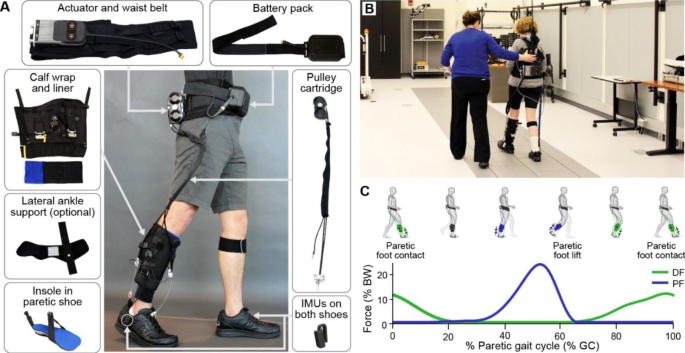
Overview of exosuit hardware and exosuit-generated assistance profile. (A) Components of a unilateral soft wearable robot (exosuit) designed to augment paretic ankle function during poststroke walking. The exosuit utilizes garment-like functional textile anchors and Bowden cables to generate assistive joint torques. Inertial measurement units (IMUs)attached to the shoe are used for online detection of gait events and system control. The system itself weighs 3.2 kg, with the different sizes of garments between 3.8 and 4.1 kg or between 3.6–8.9% (mean: 5.7%) of the subject’s body mass. Less than 14% of this mass was worn distally. (B) Study participant wearing the portable soft exosuit in the motion capture lab. (C) Example average exosuit forces from one participant. The exosuit generates plantarflexion (PF, blue) and dorsiflexion (DF, green) forces that are designed to restore the paretic limb’s contribution to forward propulsion during push-off and ground clearance, respectively
Our previous results indicate that baseline comfortable walking speed, a common clinical prognostic measure and predictor of intervention success, may impact the user’s ability to leverage exosuit assistance [19, 21, 23]. Therefore, the present study evaluates differences between people poststroke with comfortable walking speeds less than 0.93 m/s (limited community ambulators) and those with comfortable walking speeds greater than 0.93 m/s (full community ambulators), based on a recently introduced cut-off for functional stroke survivor groups [54]. Finally, the present study performs a thorough biomechanical evaluation, including effects on walking stability, control of foot landing, and slacking of the plantarflexor muscles. We hypothesize that the assistance provided by the updated portable exosuit will increase overground walking speed compared to walking without an exosuit by improving paretic ground clearance, foot landing, and propulsion. We expect these results to be enhanced in slower, more functionally limited participants. We further hypothesize that exosuit assistance will reduce the energy cost of transport, increase walking stability, and prevent plantarflexor muscle slacking.
More at link.
No comments:
Post a Comment