Wow, lot of words but couldn't make heads or tails if a protocol was in there someplace. So useless.
Association between intensive blood pressure lowering and stroke-free survival among patients with and without Diabetes
Scientific Reports volume 14, Article number: 21551 (2024)
Abstract
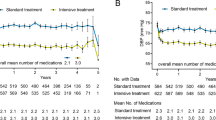
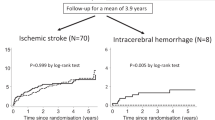
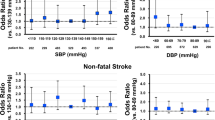
This study pooled data from SPRINT (Systolic Blood Pressure Intervention Trial) and ACCORD-BP (Action to Control Cardiovascular Risk in Diabetes Blood Pressure) trial to estimate the treatment effect of intensive BP on stroke prevention, and investigate whether stroke risk score impacted treatment effect. Of all the potential manifestations of the hypertension, the most severe outcomes were stroke or death. A composite endpoint of time to death or stroke (stroke-free survival [SFS]), whichever occurred first, was defined as the outcome of interest. Participants without prevalent stroke were stratified into stroke risk tertiles based on the predicted revised Framingham Stroke Risk Score. The stratified Cox model was used to calculate the hazard ratio (HR) for the intensive BP treatment. 834 (5.92%) patients had SFS events over a median follow-up of 3.68 years. A reduction in the risk for SFS was observed among the intensive BP group as compared with the standard BP group (HR: 0.76, 95% CI: 0.65, 0.89; risk difference: 0.98([0.20, 1.76]). Further analyses demonstrated the significant benefit of intensive BP treatment on SFS only among participants having a high stroke risk (risk tertile 1: 0.76 [0.52, 1.11], number needed to treat [NNT] = 861; risk tertile 2: 0.87[0.65, 1.16], NNT = 91; risk tertile 3: 0.69[0.56, 0.86], NNT = 50). Intensive BP treatment lowered the risk of SFS, particularly for those at high risk of stroke.
Similar content being viewed by others
Introduction
Elevated blood pressure (BP) has been identified as the major modifiable risk for stroke development with an estimated population-attributable risk of 48%1. Thus, strict and aggressive BP lowering is deemed the most important prevention strategy for both primary and secondary stroke prevention2,3,4,5. A significant benefit of intensive BP lowering the risk of stroke was observed in the ACCORD-BP trial (Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial)6. On the contrary, this treatment benefit was not found in the SPRINT (Systolic Blood Pressure Intervention Trial) trial with a similar study design but a larger sample size in comparison to the ACCORD-BP trial7.
Although this observed difference could be attributed to the trial population or the study power, treatment heterogeneity on all-cause mortality from the two trials should be otherwise noted. We observed a significant reduction in death from any cause in the SPRINT trial, which contrasted with the ACCORD-BP trial6,7. Clearly, it is known that the occurrence of death would preclude the observation of a stroke. As such, further analyses are needed to account for the presence of this terminal competing risk. Meanwhile, many researchers have identified that individual patients vary from one another in many ways that can affect the potential for benefit, which cannot be captured by conventional one-variable-at-a-time subgroup analyses8,9,10. However, the heterogeneity of treatment effect (HTE) of intensive BP lowering based on individual stroke risk has not been explored.
As such, the aims of this study were (1) to estimate the treatment effect of intensive BP lowering on stroke prevention using the pooled patient data of SPRINT and ACCORD-BP after considering the presence of competing risks from death; (2) to further investigate whether stroke risk score was associated with differential treatment effect.
No comments:
Post a Comment