http://www.uhn.ca/corporate/News/Pages/UHN_researcher_genetic_basis_formation_of_abnormal_blood_vessels_brain.aspx?
Main Page Content
1/4/2018
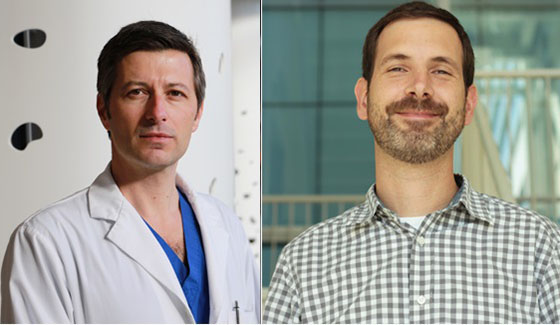
New
research by Drs. Ivan Radovanovic (L) and Jason Fish identifies a
possible genetic mutation that causes brain arteriovenous malformations
and could lead to treatment for the illness. (Photo: UHN)
The reasons why malformations occur in blood vessels remain a mystery, but it’s a fact that sometimes, in this carefully orchestrated process, things can go wrong.
The result is an Arteriovenous Malformation (AVM), an abnormal tangle of poorly formed blood vessels. AVMs can occur anywhere in the body, but are of particular concern when they occur in the brain because of the damage they can cause if they bleed or rupture.
There are different types of Brain Arteriovenous Malformations (BAVMs) and some rare forms occur in patients with inherited genetic disorders. However, most occur randomly in the population, known as sporadic BAVMs, and these generate more questions than answers.
So what causes this type of sporadic malformation? How do the many arteries and veins that make up blood vessels spontaneously start to tangle?
There have been many theories, but the genetic cause was unknown until now.
In a study published in the New England Journal of Medicine, Dr. Ivan Radovanovic from the Krembil Research Institute, Dr. Jason Fish from the Toronto General Hospital Research Institute, their research teams, and collaborators in Switzerland and Finland, identified, for the first time, a genetic basis for the formation of these abnormal blood vessels that are the leading cause of hemorrhagic stroke – bleeding in the brain – in young adults and children.
"We think that sporadic BAVMs are not present from birth but occur sometime after," says Dr. Radovanovic a neurosurgeon and scientist and co-principal investigator of the study.
"Identifying the mutations that cause this disease and showing that they only occur in the abnormal vessels forming the BAVM, but are not present in other cells of the patients body, allows us to understand how BAVMs are formed and why they are not inherited.
"This discovery also establishes therapeutic targets to treat BAVMs," he continues. "The next step will be to test drugs in the laboratory and in pre-clinical models that reverse the effect of these mutations in brain vessels. In the future, we may envision clinical trials that will test drugs that can help manage this condition in patients."
Though BAVMs are rare – occurring in roughly one per cent of the population – their inherent risk of bleeding is high over a patient's lifetime, which is a dangerous characteristic considering BAVMs often go undetected for many years. If they do bleed, they can cause permanent damage in the brain. Approximately 50 per cent of BAVMs that bleed can result in permanent disability or death.
"Even if they don't bleed, AVMs can cause seizures or other stroke-like symptoms," says Dr. Radovanovic. "Furthermore, in some cases, patients aren't always good candidates for the few treatments that are available, such as surgery, embolization or radiation.
"So it's really a condition that demands other options, and understanding its cause will open the door to other possibilities."
To identify the mutation, Dr. Radovanovic and his research team began by performing exome sequencing on the DNA from BAVM tissue that had been removed surgically as part of standard treatment for the condition. Exome sequencing is a technique to read all the protein-coding genes in a genome – the patient's DNA.
The process showed the genetic changes occurred in a gene known as KRAS. Dr. Fish and his research team then showed expression of mutant KRAS alters signalling pathways that in turn disrupt the normal migratory behaviour of endothelial cells – the cells that form the inside lining of blood vessels.
These altered cellular behaviours may be a key feature for BAVMs to develop. The mutation was found in over 60 per cent of the 72 patients with abnormal blood vessels in the brain that were part of the multi-centre study.
Interestingly, the study also identifies this same mutation/activation pathway as a potential target for drug therapy. As KRAS mutations have been shown to be involved in many cancers, such as colorectal, lung and pancreatic cancers, existing cancer drugs developed to inhibit this mutation could be tested as a possible treatment.
“These findings are really the foundation of many possibilities to better understand, manage and treat BAVMs,” says Dr. Fish. “It’s a very exciting time in this area of research.”
No comments:
Post a Comment