Interesting, but the thumb does not seem to be part of the therapy. That's a mistake that the mentor should have caught. The rest of the paper has 3 references to the thumb so maybe the pictures chosen were incorrect.
Three-Dimensional Magnetic Rehabilitation, Robot-Enhanced Hand-Motor Recovery after Subacute Stroke: A Randomized Controlled Trial
1
Department of Electronics & Information Engineering, Korea University, Sejong 30019, Republic of Korea
2
Department of Electronics Convergence Engineering, Wonkwang University, Iksan 54538, Republic of Korea
3
Department of Rehabilitation Medicine, Soonchunhyang University Cheonan Hospital, Cheonan 31151, Republic of Korea
4
Department of Regenerative Medicine, College of Medicine, Soonchunhyang University, Cheonan 31151, Republic of Korea
*
Author to whom correspondence should be addressed.
Brain Sci. 2023, 13(12), 1685; https://doi.org/10.3390/brainsci13121685
Original submission received: 10 November 2023
/
Revised: 2 December 2023
/
Accepted: 6 December 2023
/
Published: 7 December 2023
(This article belongs to the Special Issue Stroke and Acute Stroke Care: Looking Ahead)
Abstract
We developed an end-effector-type rehabilitation
robot that can uses electro- and permanent magnets to generate a
three-way magnetic field to assist hand movements and perform
rehabilitation therapy. This study aimed to investigate the therapeutic
effect of a rehabilitation program using a three-dimensional (3D)
magnetic force-based hand rehabilitation robot on the motor function
recovery of the paralyzed hands of patients with stroke. This was a
double-blind randomized controlled trial in which 36 patients with
subacute stroke were assigned to intervention and control groups of 18
patients each. The intervention group received 30 min of rehabilitation
therapy per day for a month using a 3D magnetic force-driven hand
rehabilitation robot, whereas the control group received 30 min of
conventional occupational therapy to restore upper-limb function. The
patients underwent three behavioral assessments at three time points:
before starting treatment (T0), after 1 month of treatment (T1), and at
the follow-up 1-month after treatment completion (T2). The primary
outcome measure was the Wolf Motor Function Test (WMFT), and secondary
outcome measures included the Fugl–Meyer Assessment of the Upper Limb
(FMA_U), Modified Barthel Index (MBI), and European Quality of Life Five
Dimensions (EQ-5D) questionnaire. No participant safety issues were
reported during the intervention. Analysis using repeated measures
analysis of variance showed significant interaction effects between time
and group for both the WMFT score (p = 0.012) and time (p
= 0.010). In post hoc analysis, the WMFT scores and time improved
significantly more in the patients who received robotic rehabilitation
at T1 than in the controls (p = 0.018 and p
= 0.012). At T2, we also consistently found improvements in both the
WMFT scores and times for the intervention group that were superior to
those in the control group (p = 0.024 and p
= 0.018, respectively). Similar results were observed for FMA_U, MBI,
and EQ-5D. Rehabilitation using the 3D hand-rehabilitation robot
effectively restored hand function in the patients with subacute stroke,
contributing to improvement in daily independence and quality of life.
1. Introduction
The
human hand is one of the most fascinating and sophisticated biological
motor systems, and its complex biomechanics and neural architecture
enable it to grasp objects of various shapes and sizes through the
coordinated motions of multiple fingers that can engage in creative and
practical activities, such as writing, drawing, and playing musical
instruments [1].
Hand function also has huge implications for performing tasks in a
person’s occupation. Greater difficulties in hand function correspond to
increased impairment in the use of assistive technology enabling
participation in academic and social activities [2]. Upper-extremity motor function impairment reportedly occurs in ≤80% of patients with stroke [3], and the extent of a patient’s upper-extremity dysfunction is determined by the degree of functional hand impairment [4].
Several rehabilitation techniques have been developed to restore
impaired hand function after stroke, including constraint-induced
movement therapy [5], repetitive transcranial magnetic stimulation [6],
and traditional occupational therapy. Although these therapies have
partially contributed to the recovery of hand function after stroke, the
complexity and versatility of the human hand pose a major challenge in
stroke rehabilitation [7].
In
light of these challenges, clinicians and researchers have begun to
actively apply robotic therapeutic techniques to patients undergoing
stroke rehabilitation. Robots used to restore motor function in the
upper limb are broadly categorized into end-effector-type robots and
exoskeletal-type robots [8].
The end-effector-type hand-rehabilitation robot is connected to the
distal part of the patient’s upper limb and can apply free-exercise
programs according to the patient’s hand-function level [8].
Exoskeletal-type hand-rehabilitation robots have the joint axes of the
robot aligned with the joint axes of the patient’s hand, and can train
specific muscles by controlling joint movements with calculated torques [9].
Robotic-assisted hand rehabilitation is often used to improve motor
function in stroke-related paralyzed hands and has shown significant
therapeutic benefits compared with conventional treatment [10,11].
Wearable robots have gained attention as they can embody motor
functions tailored to various hand movements by collecting motion data
or physiological signal data on the user’s hand movements through
device-mounted sensors [12]. These robots also reportedly have a positive effect on hand motor function recovery in patients with stroke [13]. Virtual-reality programs are additionally applied to improve patient compliance with the robot [14],
and hand-rehabilitation robots are being developed with artificial
intelligence technology to provide a variety of patient-specific
protocols [15].
We
have noted that magnetic forces can be efficiently used to assist the
strength of hands paralyzed by stroke and to perform exercise therapy.
Magnetic forces are invisible and can give patients the sensation that
their fingers are actually moving, which can reduce resistance to
treatment [16].
Moreover, the advantage of magnetic forces is that they can implement a
variety of finger movements in different directions based on the
magnetic force direction, regardless of the position of the hand [7].
We previously developed a three-dimensional (3D) hand-rehabilitation
robot that can perform finger-rehabilitation training with constant
force and orientation regardless of hand position and confirmed the
short-term therapeutic effect in an earlier study [17].
However, we were still uncertain if the 3D hand-rehabilitation robot
could contribute to the long-term recovery of hand function in patients
with stroke. Therefore, this study aimed to investigate the long-term
effects of a 3D hand-rehabilitation robot on the recovery of hand
function in patients with stroke-related hand paralysis.
2. Materials and Methods
2.1. Magnetic Force-Driven Hand-Rehabilitation Robot
A
developed electromagnetic rehabilitation system with multilink magnetic
devices on the fingers can create and induce flexion and extension
movements of the fingers because the applied alternating current (AC)
magnetic field generates magnetic forces (attraction and repulsion) [16].
These forces create a bending or extending motion of the fingers. The
magnetic force required to move the finger the desired amount is
controlled by the amount of current flowing through the coils [18].
The 3D hand-rehabilitation systems with magnetic multilink devices have
the advantage of being able to detect finger positions in real time,
enabling active flexing and extending regardless of the hand position (Figure 1).
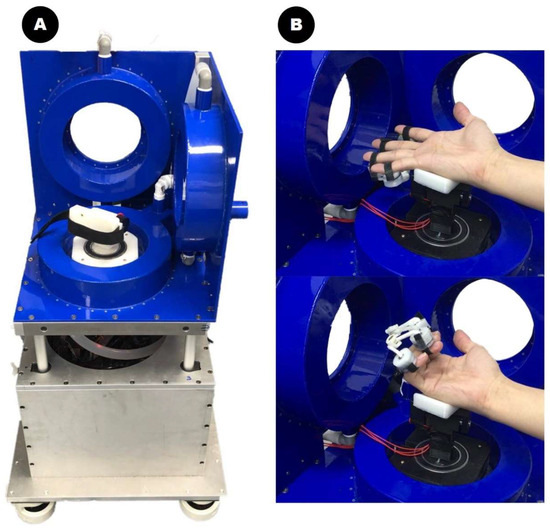
Figure 1.
The three-dimensional magnetic force-driven finger-rehabilitation robot is shown. (A) The developed magnetic array device. (B)
The extension and flexion movements of the hand aided by magnetic
forces in the device. The magnetic array placed on the patient’s finger
generates attraction and repulsive forces driven by the magnetic field
of the three-dimensional coil system. These magnetic forces are used to
move the paralyzed fingers of patients with stroke.
Because patients with stroke cannot remain
immobilized for long periods of time, their finger positions are
constantly changing. Therefore, the change in angle is fed back to the
coil’s current controller, and the direction of the magnetic field is
automatically changed by the control algorithm to match the hand
position. The robot can effectively perform finger-rehabilitation
exercises by applying a constant external force to the patients fingers
at all times, regardless of the patient’s hand position. More details
about the magnetic force-based hand-rehabilitation robot’s mechanism are
presented in a previous paper [17].
2.2. Study Design
The
study included patients with ≥grade 2 finger motor grade by manual
muscle test on the paralyzed side after stroke. The patients’ ages
ranged from ≤20–80 years. Stroke onset had occurred ≤3 months before
study inclusion for all patients. The patients with spasticity or severe
muscle shortening of a modified Tardieu Scale grade ≥3, patients with
severe cognitive impairment who were unable to understand the
physiotherapist’s instructions, maintain a sitting position, and receive
appropriate rehabilitation due to serious medical conditions, such as
pneumonia, were excluded from the study.
This
was a parallel-group, single-blind, randomized controlled trial (Unique
identifier: KCT0007970) with participants randomly assigned in a 1:1
ratio between the treatment and placebo groups. A block randomization
process to ensure equal numbers in each treatment group was used by a
statistician to achieve randomization before starting the trial. The
participants were randomly assigned to the intervention and control
groups.
The intervention was designed so that
the control and experimental groups received the same amount of
rehabilitation time. Patients of intervention and control groups equally
received occupational therapy to restore upper limb function for 1 h a
day. Specifically, the patients in the control group received
conventional occupational therapy, including the upper-extremity range
of motion exercises, finger stretching, sensory stimulation, and
strengthening exercises for one hour once a day. The patients in the
intervention group received conventional occupational therapy for 30
min, followed by magnetic force-driven robotic hand rehabilitation
therapy for the remaining 30 min a day.
Physical
therapy programs such as neurodevelopmental therapy, muscle
strengthening exercises, and gait training, which are generally
administered to stroke patients, were performed equally for both groups
for an hour per day.


No comments:
Post a Comment