But didn't your competent? doctor immediately prescribe statins to help in your recovery?
Or don't you have a functioning stroke doctor who incompetently missed this research from 2011?
1. Statins.
tested in rats from 2003
http://Statins induce angiogenesis, neurogenesis, and synaptogenesis after stroke Statins induce angiogenesis, neurogenesis, and synaptogenesis after stroke
Simvastatin Attenuates Stroke-induced Splenic Atrophy and Lung Susceptibility to Spontaneous Bacterial Infection in Mice
Or,
Simvastatin attenuates axonal injury after experimental traumatic brain injury and promotes neurite outgrowth of primary cortical neurons
October 2012
tested in humans, March, 2011
http://www.medwirenews.com/39/91658/Stroke/Acute_statin_therapy_improves_survival_after_ischemic_stroke.html
And now lost even to the Wayback Machine
So I think this below is the actual research;
Association Between Acute Statin Therapy, Survival, and Improved Functional Outcome After Ischemic Stroke April 2011
The latest here:
Statins and cognitive decline in patients with Alzheimer’s and mixed dementia: a longitudinal registry-based cohort study
Alzheimer's Research & Therapy volume 15, Article number: 220 (2023)
Abstract
Background
Disturbances in brain cholesterol homeostasis may be involved in the pathogenesis of Alzheimer’s disease (AD). Lipid-lowering medications could interfere with neurodegenerative processes in AD through cholesterol metabolism or other mechanisms.
Objective
To explore the association between the use of lipid-lowering medications and cognitive decline over time in a cohort of patients with AD or mixed dementia with indication for lipid-lowering treatment.
Methods
A longitudinal cohort study using the Swedish Registry for Cognitive/Dementia Disorders, linked with other Swedish national registries. Cognitive trajectories evaluated with mini-mental state examination (MMSE) were compared between statin users and non-users, individual statin users, groups of statins and non-statin lipid-lowering medications using mixed-effect regression models with inverse probability of drop out weighting. A dose-response analysis included statin users compared to non-users.
Results
Our cohort consisted of 15,586 patients with mean age of 79.5 years at diagnosis and a majority of women (59.2 %). A dose-response effect was demonstrated: taking one defined daily dose of statins on average was associated with 0.63 more MMSE points after 3 years compared to no use of statins (95% CI: 0.33;0.94). Simvastatin users showed 1.01 more MMSE points (95% CI: 0.06;1.97) after 3 years compared to atorvastatin users. Younger (< 79.5 years at index date) simvastatin users had 0.80 more MMSE points compared to younger atorvastatin users (95% CI: 0.05;1.55) after 3 years. Simvastatin users had 1.03 more MMSE points (95% CI: 0.26;1.80) compared to rosuvastatin users after 3 years. No differences regarding statin lipophilicity were observed. The results of sensitivity analysis restricted to incident users were not consistent.
Conclusions
Some patients with AD or mixed dementia with indication for lipid-lowering medication may benefit cognitively from statin treatment; however, further research is needed to clarify the findings of sensitivity analyses.
Background
The brain houses about a quarter of the cholesterol present in the body, making it the richest cholesterol-containing organ [1]. The essential role of brain cholesterol is reflected in its involvement in numerous physiological processes such as maintaining membrane integrity, neurotransmission and synaptogenesis [2]. A dysregulation of brain cholesterol homeostasis may be involved in the pathogenesis of Alzheimer’s disease [2] through interference with the amyloidogenic Aβ pathway [3], impairment of cerebral blood flow [4], and other mechanisms [5]. On the other hand, the association of peripheral hypercholesterolemia and cognition is complex. Peripheral hypercholesterolemia in midlife has been linked to cognitive decline and AD in late-life [6, 7] through different mechanisms [7,8,9,10]. Moreover, genetic polymorphism of brain cholesterol transporter ApoE4 and several additional genetic factors implicated in lipid metabolism could be relevant to AD pathogenesis [11, 12]. In contrast, peripheral hyperlipidaemia in late life is a marker of a better general health and cognition [13, 14].
The possible cognitive effects of HMG-CoA reductase inhibitors or statins, which are used in cardiovascular disease prevention, have sparked extensive research in the last few decades. Based on their pharmacokinetic characteristics, statins can be divided according to their structure (fungus-derived or synthetical), lipophilicity, metabolism, bioavailability, potency and binding to different proteins and transporters [15]. The multi-layered effects of statins on cognition are translated through numerous neurodegenerative processes in a cholesterol-dependent as well as independent (´´pleiotropic´´) manner [15, 16]. Statins seem to interfere with the amyloidogenic cascade [17] and phosphorylation of tau [18], provide beneficial vascular factors through endothelial function and clearance of neurotoxic substances [19], decrease neuroinflammation and oxidative stress as well as promote neuronal survival and plasticity, synaptogenesis and neurotransmission [16].
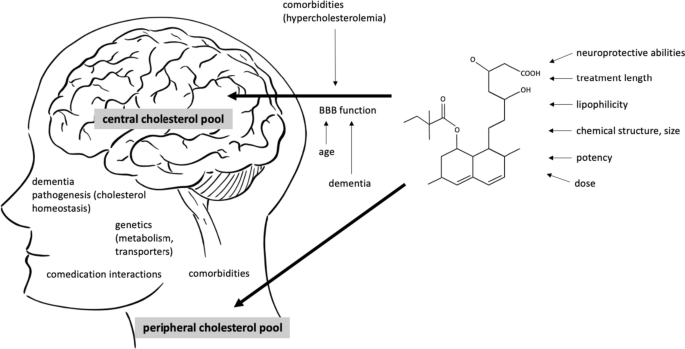
The overall cognitive effects of statins are likely connected to a complex interaction of factors, related to the patient’s characteristics, integrity of blood–brain barrier permeability [20], characteristics of statins [18], time of treatment, dosages as well as critical time windows in the pathogenesis of dementia [21, 22] (Fig. 1).
Interaction between the patient’s and medication’s characteristics potentially influence the cognitive effects of statins. Two separate cholesterol pools in the body are thought to be connected to the risk of Alzheimer’s disease (AD), central and peripheral. The brain penetration of statins has been attributed to different factors linked to BBB crossing (lipophilicity of a statin, chemical structure, molecular weight and size of the molecule, different transporters and their genetic polymorphisms). The structure of the barrier itself additionally influences the permeability of statins and is affected by aging, neurodegenerative processes and possibly, peripheral hypercholesterolemia. The overall cognitive effects of statins are likely a result of their central and peripheral actions and are connected to the time of intervention in life and the pathogenesis of AD. Moreover, an interaction of comorbidities and comedication, a sufficient time of treatment and dosages are important. In midlife, protective effect of statins against AD could be achieved through lowering the metabolic risk of hyperlipidaemia. BBB blood–brain barrier, AD Alzheimer’s disease
Despite the extensive number of observational cohort studies and some clinical trials on statins, their ability to prevent dementia or ameliorate cognitive decline after disease onset is still unclear. A number of mild and reversible short-term cognitive adverse effects [23, 24] contributed to a warning for the labelling of statins by the US Food and Drug Administration. However, numerous large systematic reviews and meta-analyses have not confirmed these adverse cognitive effects [25,26,27,28,29] and some suggested that the use of statins may lower the risk of AD [25, 30,31,32,33]. Clinical trials generally reported a null effect [34,35,36] but were commonly underpowered or used less robust cognitive evaluation tools. Comparably less information is available regarding the effect of statins on cognitive decline in patients with established AD [37,38,39,40]. Epidemiological biases inherent to observational design or a heterogeneous design of studies partly explain these discrepancies [41].
The aim of our study was to evaluate the association between statin use and cognitive decline over time in a large cohort of patients diagnosed with AD or mixed AD dementia. We hypothesized that statins that cross the BBB would be associated with less cognitive decline evaluated with mini-mental state examination (MMSE) in these patients.
No comments:
Post a Comment