Written in 2009, did your hospital do ANYTHING AT ALL with it?
Performance adaptive training control strategy for recovering wrist movements in stroke patients: a preliminary, feasibility study
Journal of NeuroEngineering and Rehabilitation volume 6, Article number: 44 (2009) Cite this article
-
8314 Accesses
-
56 Citations
-
3 Altmetric
Abstract
Background
In the last two decades robot training in neuromotor rehabilitation was mainly focused on shoulder-elbow movements. Few devices were designed and clinically tested for training coordinated movements of the wrist, which are crucial for achieving even the basic level of motor competence that is necessary for carrying out ADLs (activities of daily life). Moreover, most systems of robot therapy use point-to-point reaching movements which tend to emphasize the pathological tendency of stroke patients to break down goal-directed movements into a number of jerky sub-movements. For this reason we designed a wrist robot with a range of motion comparable to that of normal subjects and implemented a self-adapting training protocol for tracking smoothly moving targets in order to facilitate the emergence of smoothness in the motor control patterns and maximize the recovery of the normal RoM (range of motion) of the different DoFs (degrees of Freedom).
Methods
The IIT-wrist robot is a 3 DoFs light exoskeleton device, with direct-drive of each DoF and a human-like range of motion for Flexion/Extension (FE), Abduction/Adduction (AA) and Pronation/Supination (PS). Subjects were asked to track a variable-frequency oscillating target using only one wrist DoF at time, in such a way to carry out a progressive splinting therapy. The RoM of each DoF was angularly scanned in a staircase-like fashion, from the "easier" to the "more difficult" angular position. An Adaptive Controller evaluated online performance parameters and modulated both the assistance and the difficulty of the task in order to facilitate smoother and more precise motor command patterns.
Results
Three stroke subjects volunteered to participate in a preliminary test session aimed at verify the acceptability of the device and the feasibility of the designed protocol. All of them were able to perform the required task. The wrist active RoM of motion was evaluated for each patient at the beginning and at the end of the test therapy session and the results suggest a positive trend.
Conclusion
The positive outcomes of the preliminary tests motivate the planning of a clinical trial and provide experimental evidence for defining appropriate inclusion/exclusion criteria.
Background
Decreased wrist range of motion (ROM) (flexion and/or extension, abduction/adduction or pronation/supination) after trauma or surgery can be a challenging problem. Physical therapy, orthoses, and additional surgical interventions may not restore the desired functionality even after an intensive rehabilitation program. Therapists spend a considerable amount of practice time in differential diagnosis of these losses and selecting appropriate intervention strategies to restore passive and active motion in concordance with the pathology and to prevent loss of range of motion after injury.
While the regular treatment for wrist stiffness is physical therapy or surgery, researchers are looking for an alternative and more efficient and automatic procedure by means of robotic applications.
Several systems for wrist rehabilitation have been developed in research centres and universities, for example RiceWrist [1]; MIME [2]; IMT3 [3], HWARD [4]; the Okayama University pneumatic manipulator [5], and the devices overviewed in [6–9]. The majority are also used for rehabilitation in health centres and hospitals, often coupled with MIT-MANUS [10], ARMIN [11], MIME, HapticMaster [12] and wire-based device from Rosati et. al. [13] for rehabilitation of proximal limb. Robot assisted therapy are primarily based on goal-directed point-to-point movement involving multiple DoFs [14]; main purpose is increasing the ROM of the paretic limb in order to regain motor abilities for the Activities of Daily Living (ADL). Contrarily regular physical therapy of wrist rehabilitation consists in a splinting treatment for each single DoF at time, and there have been many studies that look at the splints' effectiveness and what type of splint would be best [15, 16]. Static progressive splinting is a time-honored concept, for more than 20 years, clinicians have recognized the effectiveness of static progressive splints to improve passive range of motion (PROM). Splint designers then sought a means to improve the technique with components that offer infinitely adjustable joint torque control and are easy to apply, lightweight, low-profile, and reasonably priced.
Dynamic splints use some additional component (springs, wires, rubber bands) to mobilize contracted joints [17–19]. This dynamic pull functions to provide a controlled gentle force to the soft tissue over long periods of time, which encourages tissue remodeling without tearing. The issues that make dynamic or static progressive splinting technically difficult include determining how much force to use, how to apply the force, how long to apply the force, and how to prevent added injury to the area. Things could change if the dynamic splinting is delivered using devices which are able to modulate torque delivering and space the range of motion.
Therefore we intend to approach the robotic therapy for wrist rehabilitation using a continuous dynamic splinting of each single DoF but contrarily to the regular progressive splinting we want also to highlight the voluntary component of movement. A performance adaptive control strategy has been developed, with the purpose of providing variable assistance by means of a general training paradigm for stroke patients.
Methods
Apparatus: the wrist device
The Wrist-Robot [20], herewith reported, has been developed at the Italian Institute of Technology with three main requirements: 1) back-drivability of the 3 DoFs (Degree of Freedom), in order to assure a smooth haptic interaction between the robot and the patient; 2) mechanical and electronic modularity, in order to facilitate the future integration into a haptic bimanual arm-wrist-hand system with up to 12 DoFs; 3) scalable software architecture. The Wrist Robot is intended to provide kinesthetic feedback during the training of motor skills or rehabilitation of reaching movements. Motivations for application of robot therapy in rehabilitation of neurological patients come from experimental studies about the practice-induced plastic reorganization of the brain in humans and animal models [21, 22].
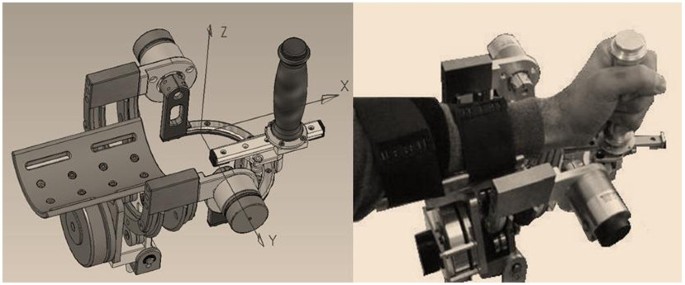
The robot (figure 1) is a 3 DOFs exoskeleton: F/E (Flexion/Extension); Ad/Ab (Adduction/Abduction); P/S (Pronation/Supina-tion).
3DoF Wrist Device. It has 3 DOFs: F/E, P/S, Ad/Ab. One motor is used for F/E and P/S; two motors for Ad/Ab.
The chosen class of mechanical solutions is based on a serial struct>ure, with direct drive by the motors: one motor for pronation/supination, one motor for flexion/extension and two parallel coupled motors for abduction/adduction that allow to balance the pronosupination rotation during motion.
The problem of measurement of arm position is thus reduced to the solution of the device kinematics, with no further transformations required, allowing to actuate the robot to control feedback to a specific human joint, for example to constrain the forearm rotation during wrist rehabilitation, without affecting other joints.
The corresponding rotation axes meet at a single point as shown in figure 1.
The subjects hold a handle connected to the robot and their forearms are constrained by velcros® to a rigid holder in such a way that the biomechanical rotation axes are as close as possible to the robot ones. Unavoidable small joints misalignments are partially reduced by means of a sliding connection between the handle and the robot and the forearm can be moved vertically in order to fit the rotation axis of the pronation/supination DoF. In order to minimize the effect of occasional compensatory shoulder/trunk movements during training exercises, the body is firmly strapped to a robust chair and the chair is positioned in such a way to have the elbow flexed about 90 deg and the hand pointing to the centre of a 21" CD screen, in correspondence with the neutral anatomical orientation of the hand.
Having in mind the general requirements of robot therapy [22, 23], we identified the following design specifications:
-
1.
sufficient level of the torque at the handle (tab. I)
-
2.
large workspace
low friction and direct drive motors enhance the back-driveability of the manipulandum, thus simplifying its control without needing a closed loop force control scheme. The mechanical range of motion (ROM) is as follows: F/E = -70° ↔ +70°; Ad/Ab = -35° ↔ +35°; P/S = -80° ↔ +80°. These values approximately match the ROM of a typical human subject (Table 1).
Each DOF is measured by means of a high-resolution encoder (2048 bits/rev) and is actuated by one or two brushless motors, in a direct-drive, back-drivable connection, providing the continuous torque values reported in table 1. The control architecture integrates the wrist controller with a bi-dimensional visual virtual reality environment (VR) for showing to the subjects the actual joint rotation transformation of the hand, the corresponding target direction and two performance indicators defined in the following. The software environment is based on Simulink® and RT-Lab®. The control architecture includes three nested control loops: 1) an inner loop, running at 7 kHz, used by the motor servos; 2) an intermediate loop, running at 1 kHz, for the low level control; 3) a slower loop, running at 100 Hz, for implementing the VR environment and the user interface. The mechanical structure of the wrist robot was designed in such a way to allow a simple and immediate mounting for patients' forearm.
Task
The task is mono-dimensional tracking of a sinusoidally moving target, using one DOF at a time: F/E, Ad/Ab or P/S, respectively; this approach is consistent with the dynamic splinting paradigm which is primarily used to regain the passive ROM after trauma or surgical intervention; the subject aims to move the handle to track the harmonic motion of the target using his/her active ROM; the robot gently intervenes if the subject is not able to actively cover the required angular displacement. Three different experiments were then carried out for the three different DoFs of the wrist. For each experiment, there was one active DoF, which received controlled assistance by the robot, while the two other DoFs were hold by the robot in a small neighbourhood of the neutral position [24–26].
In order to make the task interesting and challenging at the same time, the level of difficulty was managed by the controller modulating two parameters as a function of the performance: a) frequency of the target motion; b) level of the robot assistance. The controller implementation is discussed and illustrated in the next section.
Results
Although the clinical states of the three subjects are rather different, as reported in table 3, all of them were able to carry out the proposed exercises in a consistent way, with different performance profiles considering the performance adaptive nature of the controller architecture. For clarity sake, in the present preliminary/feasibility study, the following figures will refer to subject S3, who is the most severely affected and therefore the worst case in the experienced population. Figure 4 shows the evolution of the frequency of the moving target for each DoF, while the ϑ o position scans through the 11 values that are uniformly placed in the corresponding ROM: 40s for each step + 4s of rest between one step and the next one. For each step, the peak value of the frequency depends on the position in the workspace of each DoF and on the specific pathological condition of each patient: the figure shows that S3 has higher difficulty in extension than flexion, in adduction than abduction, and in pronation than supination.
More at link.
No comments:
Post a Comment