Ask your doctor to ensure human testing of this in stroke subjects to see if this would help stroke recovery. Doesn't do that, you don't have a functioning stroke doctor.
Exploring the neuroprotective potential of cell-penetrating peptides, extracellular vesicles, and micro ribonucleic acids
In a recent review published in Biomedicines, researchers explored extracellular vesicles (EVs), cell-penetrating peptides (CPPs), and micro ribonucleic acids (miRNAs) as therapies for neurodegenerative diseases, such as Alzheimer’s disease (AD) and Parkinson’s disease (PD).
Background
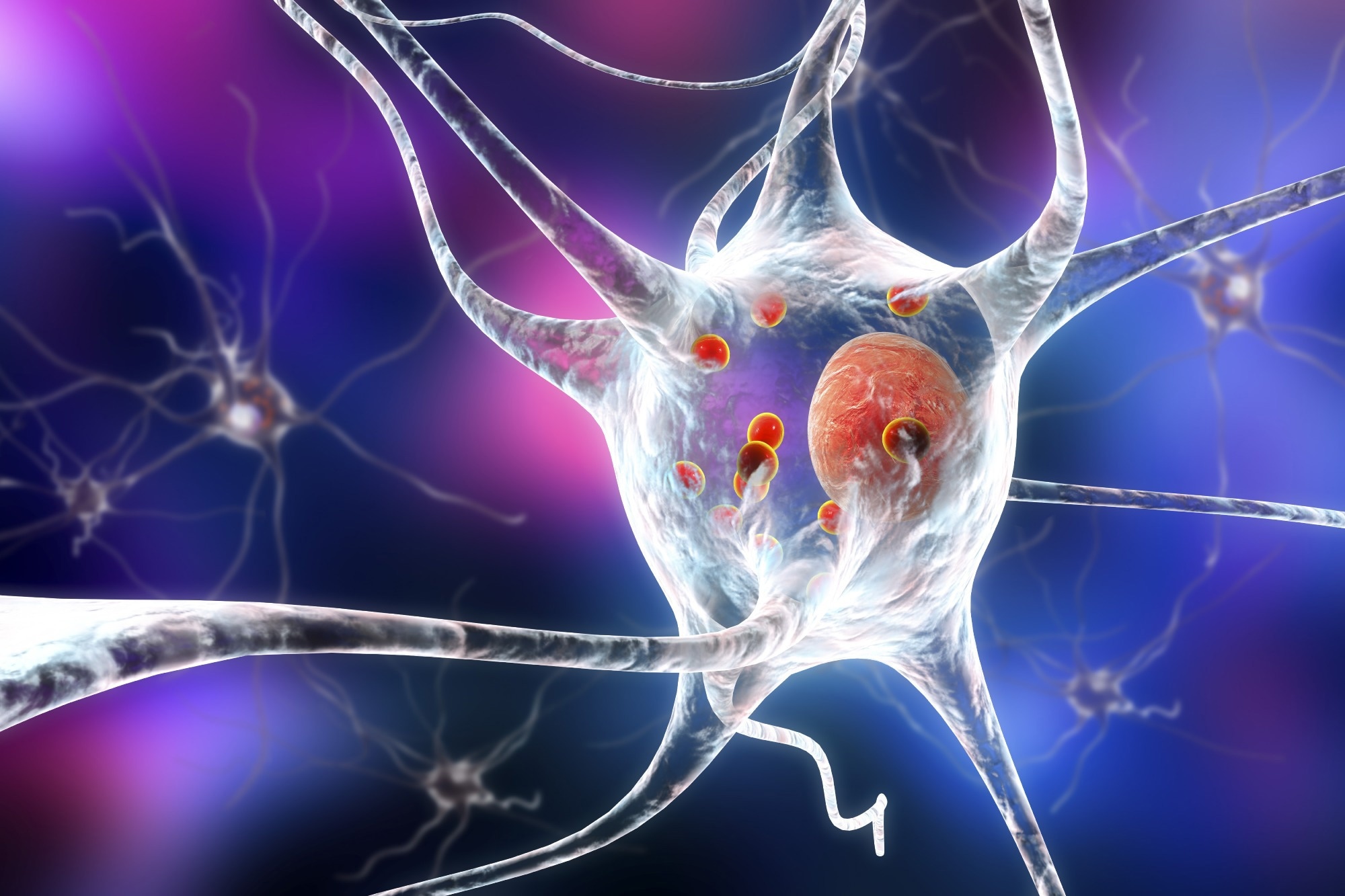
Neurodegenerative diseases such as AD and PD are characterized by the progressive loss of dopaminergic neurons with significant protein accumulation in the brain. They are among the leading causes of death globally. PD usually presents with muscular rigidity, bradykinesia, and tremors, whereas AD patients develop confusion and dementia. Existing therapies include various pharmaceutical, physical, and surgical options. However, the treatments do not modify disease and may fail due to a lack of blood-brain barrier (BBB)-crossing abilities, warranting novel neuroprotective therapies.
About the review
In the review, researchers presented EVs, CPPs, and miRNAs as neuroprotective therapeutics for AD and PD patients.
Pathophysiological mechanisms of AD and PD and existing therapeutics
Profound neurodegeneration is observed in PD and AD with overlapping mechanisms, including the accumulation of α-synuclein and Tau proteins, shared mutations such as PTEN-induced kinase 1 (PINK1), amyloid precursor protein (APP), and leucine-rich repeat kinase 2 (LRRK2). In addition, PD pathophysiology includes defects in the DJ-1 and parkin genes.
In both diseases, changes in autophagy and lysosomal pathways are observed, impairing the clearance of protein aggregates. Neurodegeneration is associated with elevated oxidative stress, synaptic toxicities, and network dysfunctions. The presence of β-amyloid plaques and tau-comprising neurofibrillary tangles are observed in AD, and Lewy bodies rich in α-synuclein are observed in PD.
Currently, Food and Drug Administration (FDA)-authorized AD treatments include N-methyl-D-aspartate (NMDA) receptor antagonists and cholinesterase inhibitors (AChEIs). The AChEIs, including donepezil, galantamine, and rivastigmine, block cholinesterase enzymes, increasing acetylcholine levels at synaptic clefts. NRRRR receptor agonists reduce calcium-associated changes and restore normal physiology, retarding AD progression. Surgical options, mainly aimed at symptomatic management, include cerebrospinal spinal fluid shunting, β-amyloid and tau protein clearance, and intraventricular infusions. Emerging therapies include nerve growth or neuroprotective factors like monosialitetrhexosylgangioside and tissue grafts.
Current PD therapies include dopamine agonists, L-DOPA, levodopa, L-3,4 dihydroxyphenylalanine, amantadine, and MAO-B inhibitors such as selegiline, to restore dopamine levels in the substantia nigra (SN). Partial NMDAR antagonists such as memantine have also been tried. Surgical options for PD include deep brain stimulation for decreasing neurofibrillary tangles, β-amyloid deposits, and Lewy bodies. Physical therapies for AD and PD include cognitive behavioral therapy, lifestyle modifications, and speech therapy to enhance mood, reduce aggression and improve strength and mobility.
Therapeutic potential of EVs, CPPs and miRNAs
Therapies are required that reduce the side effects of pharmaceutical drugs, target particular pathways, restore neuronal losses as well as protect against further neurodegeneration. Recent research has indicated the use of stem cells, EVs, CCPs miRNAs, and nanoparticles, for treating neurodegeneration.
EVs, derived from mesenchymal stromal cells, carry genomic information or deliver small molecules locally or systemically and can eradicate disease and also deliver next-generation therapeutics. EVs have been used to reduce oxidative stress, protein accumulation, pro-inflammatory cytokine expression, and associated neurodegeneration. EV drawbacks include cellular target specificity and the inability to cross the BBB.
CPPs are positively charged, short sequences of amino acids that can cross the BBB, and penetrate the cornea and skin. CPPs could translocate nucleic acids and other molecules across cellular membranes. The use of CPPs has reduced protein aggregation and neuroinflammation, and improved mitochondrial function, restoring functional synapses. CPPs have low cellular selectivity and transport efficacy but can be combined with EVs, harnessing the natural delivery ability of EVs. In addition, CPPs have poor chemical stability and can be degraded by enzymes, reducing their potency.
Micro RNAs are non-coding, small RNAs, that can mediate cell-to-cell communication and regulate post-transcriptional gene expression of L1CAM, APP, and caspase genes to reduce neurodegeneration. In addition, miRNAs such as miR-23a can detect cognitive impairments in AD, and altered levels of miR-185-5p and miR-30a-5p are observed in PD.
Upregulating miR-34a expression is associated with lowered tau protein synthesis, and miR34b/c levels can regulate the parkin and DJ-1 genes in PD. Studies have reported that miRNA 124-3p-enhanced EVs protected SN neurons from neurodegeneration associated with increased oxidative stress and superoxide generation. Limitations for miRNA use include low tissue specificity. Modifying CPPs on EV surfaces to increase arginine enrichment could enhance cell penetration and enable BBB crossing for targeted neuroprotective actions using miRNAs.
Based on the review findings, next-generation neuroprotective therapeutics could be formulated by combining EVs, CCPs, and miRNAs for enhanced neuroprotection and restoration of neurological functions in AD and PD.
- Keighron, C.N.; Avazzadeh, S.; Goljanek-Whysall, K.; McDonagh, B.; Howard, L.; Ritter, T.; Quinlan, L.R. (2023). Extracellular Vesicles, Cell-Penetrating Peptides and miRNAs as Future Novel Therapeutic Interventions for Parkinson’s and Alzheimer’s Disease. Biomedicines. doi: https://doi.org/10.3390/ biomedicines11030728 https://www.mdpi.com/2227-9059/11/3/728

No comments:
Post a Comment