Is your competent? doctor closely following this because of your risk of Parkinsons post stroke? NO? So, you DON'T have a functioning stroke doctor, do you?
Parkinson’s Disease May Have Link to Stroke March 2017
The latest here:
How Neurons Decline as Parkinsons Develops
Electrical activity dwindles in cells long before movement issues become visible.
It’s an unsettling thought: You could be walking around for 20 years developing Parkinson’s disease and not even know it.
And once symptoms appear, it’s too late for a cure.
What if a therapy that treats the root causes of Parkinson’s, not just the symptoms, could be started earlier?
Researchers in the School of Medicine at The University of Texas Health Science Center at San Antonio are studying changes in Parkinson’s-affected cells at various stages of the disease, long before any symptoms are evident. They describe the changes in an April issue of the Journal of Neuroscience.
The hope of the research is twofold: 1) gain understandings that can be used to formulate a drug to arrest the disease at a halfway point, and 2) lengthen the time when patients with Parkinson’s can lead healthy, productive lives.
Hidden changes
“For the first time we are getting a look at what’s going on in the time window before the disease visibly takes hold but while changes are occurring,” said study senior author Michael Beckstead, Ph.D., assistant professor of physiology and a member of the Barshop Institute for Aging and Longevity Studies at the UT Health Science Center.
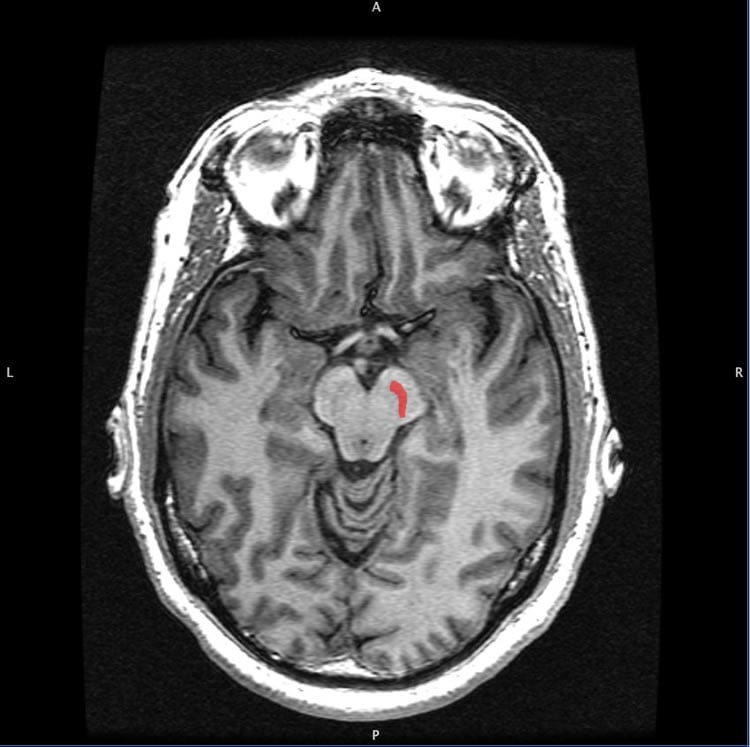
Parkinson’s is marked by the degeneration and death of cells called dopamine neurons. These neurons are found in a brain structure called the substantia nigra. The Health Science Center researchers studied mice in which only these neurons are affected by a genetic mutation.
The MitoPark mouse, as it is called, is designed so that mitochondrial activity is hampered just in dopamine neurons of the substantia nigra. Mitochondria produce energy for our cells, and since these mice have impaired mitochondria, their dopamine neurons don’t make energy efficiently.
Mimics human Parkinson’s
At first, the mice are completely normal, but as weeks and months go by, the mutation causes their dopamine neurons to slowly become sick and die off. “It’s a progressive model in that these changes don’t take place overnight,” Dr. Beckstead said. “This makes it like the human disease, which is thought to be somewhere in the range of a 20-year process before symptoms become evident.”
In MitoPark mice, behavioral symptoms such as tremor start to manifest when the mice are about 20 weeks old. The UT Health Science Center study assessed functional status at time points before that — comparing dopamine neuron function at 6-10 weeks of age with function at 11-15 weeks of age and function at 16-plus weeks.
Timeline of decline
With
these comparisons, the researchers constructed a timeline of functional
decline in the dopamine neurons. They observed changes in three
categories:
- Smaller dopamine neurons
- Reduced communication between the neurons
- Impaired electrical activity of the neurons
“Pretty much everything we measured declined in these cells,” Dr. Beckstead said. “It was really remarkable how everything we studied changed. It was a general decline, and these changes were all occurring before the animals were symptomatic, before you could detect any sort of deficit in their movement.”
In older mice starting to display the abnormal movements of the disease, the scientists made another observation — heightened gene expression to increase the electrical activity in the dopamine neurons.
“This is a late occurrence in the disease process,” Dr. Beckstead said. “We believe the cells are trying to compensate for the declining electrical activity. That’s probably how humans are able to be free of symptoms for so long when they have Parkinson’s, even though 30 percent or more of their dopamine neurons have died out.”
The study results aren’t going to translate into a clinical therapy any time soon, but such findings offer the promise that one day the root cause of Parkinson’s may be understood and treated.
Current treatments for Parkinson’s disease are all symptomatic. They focus on improving the movement deficits and making the patients more comfortable.
“We don’t have any treatments right now that actually affect the disease process,” Dr. Beckstead said. “The reason we don’t have any is we don’t understand what’s going on in the early stages of this disease. Studies such as ours will help fill in those knowledge gaps.”
Funding: Grants from the William and Ella Owens Medical Research Foundation, the National Institutes of Health and the U.S. Department of Veterans Affairs supported this work.
Source: Will Sansom – UT Health Science Center San Antonio
Image Credit: The image is credited to Geoff B Hall and is in the public domain.
Original Research: Abstract
for “Dopaminergic Neurons Exhibit an Age-Dependent Decline in
Electrophysiological Parameters in the MitoPark Mouse Model of
Parkinson’s Disease” by Sarah Y. Branch, Cang Chen, Ramaswamy Sharma,
James D. Lechleiter, Senlin Li, and Michael J. Beckstead in Journal of Neuroscience. Published online April 6 2016 doi:10.1523/JNEUROSCI.1395-15.2016
No comments:
Post a Comment