With all this earlier research our researchers should be able to put this all together and create real human brains that can be damaged by stroke and show how to stop and reverse such damage. But that is way too pie in the sky for our stroke medical professionals to understand and implement.
Multiregional brain on a chip Jan 2017
Draper Laboratory developing “Brain-on-a-Chip” October 2012
"Alzheimer's-in-a-Dish" Docs Win Top Smithsonian Ingenuity Award Nov. 2015
A patient’s budding cortex — in a dish? June 2015
Cell cultures in petri dishes open new doors to brain research April 2017
The latest here:
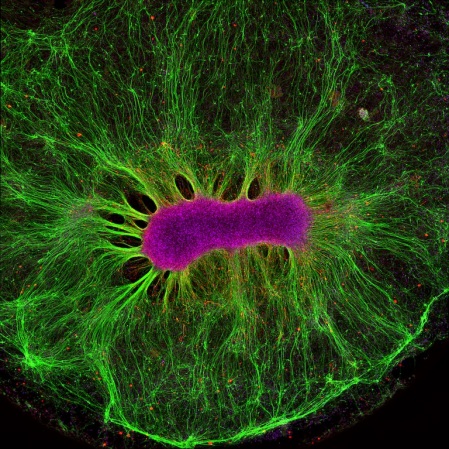
Something pretty incredible happens—both visually and scientifically—when researchers spread neural stem cells onto a gel-like matrix in a lab dish and wait to see what happens. Gradually, the cells differentiate and self-assemble to form cohesive organoids that resemble miniature brains!
In this image of a mini-brain organoid, the center consists of a clump of neuronal bodies (magenta), surrounded by an intricate network of branching extensions (green) through which these cells relay information. Scattered throughout the mini-brain are star-shaped astrocytes (red) that serve as support cells.
Collin Edington and Iris Lee created this striking image in Linda Griffith’s lab at Massachusetts Institute of Technology (MIT), Cambridge. While it looks like a single image, the picture actually took about 12 hours to produce, using a confocal laser scanning microscope to zoom in and capture the microscopic details, pixel by pixel, before digitally stitching the series of images all together. For their painstaking efforts, the team was one of 10 winners in the 2017 Koch Institute Image Awards at MIT, established to recognize and publicly display extraordinary works of art and science.
One of the things that fascinated Edington and Lee about this particular mini-brain was its surprisingly organized structure, which emerged over the course of about two weeks. In fact, one of the most interesting aspects of growing organoids in the lab is that by simply changing the chemical makeup and physical consistency of the hydrogel on which the stem cells are placed, it is possible to influence the ways in which they differentiate and assemble. This enables researchers to tinker with and fine-tune the gel’s characteristics to encourage cells to take on different forms. It also reveals a critical component of the development of complex organs—the cellular environment really matters.
In the experiment captured in this image, the researchers randomly seeded thousands of neural stem cells from human embryonic stem cell lines into a dime-sized well on a standard laboratory plate. Those cells divided and differentiated into hundreds of thousands of cells to form the mini-brain organoid shown above. By studying these mini-brains in the lab, researchers can explore the way a “typical” organoid functions, as well as learn what goes wrong in organoids generated from induced pluripotent stem cells derived from people affected by Alzheimer’s disease or other brain conditions.
Griffith’s lab isn’t stopping with the brain. In fact, this mini-brain is part of a much larger project, funded by NIH and Defense Advanced Research Projects Agency, to produce many different types of “mini-organs”—representing the liver, gut, lung, heart, and more. The goal is to link the individual organoids together to form a “human on a chip.” That integrated approach is important because organs don’t act in isolation in either health or sickness.
Alzheimer’s disease is a good example. While it’s primarily a disease of the brain, it has become increasingly clear that the gut and liver play a role, too. The “human on a chip” platform will make it possible to study such complex interactions in Alzheimer’s disease and many other conditions in the lab, with the ultimate goal to accelerate development of safe and effective new treatments.
Links:
Griffith Lab (MIT, Cambridge, MA)
Human Physiome on a Chip (MIT)
Meet Chip (National Center for Advancing Translational Sciences/NIH)
NIH Support: National Center for Advancing Translational Sciences
No comments:
Post a Comment