Your competent? doctor has had a treatment protocol for this for over a decade? Right? Oh no, you DON'T have a functioning stroke doctor, do you? And your board of directors is so incompetent they don't fire incompetent doctors?
Psoriasis: an emerging risk factor for ischemic stroke?
- 1Department of Neurology, Medical University of Warsaw, Warsaw, Poland
- 2Chair and Department of Experimental and Clinical Physiology, Laboratory of Centre for Preclinical Research, Medical University of Warsaw, Warsaw, Poland
- 3Department of Pathology, Medical University of Warsaw, Warsaw, Poland
In 2020 nearly 12 million people worldwide suffered a stroke, and acute ischemic stroke (AIS) is the most frequent stroke subtype, accounting for approximately 65% of total stroke incidence. Therefore, primary prevention, including non-traditional risk factors, should be recognized as a major public health priority. Research has shown that autoimmune diseases associated with chronic systemic inflammation, such as psoriasis, are commonly linked to AIS incidence. Psoriasis is a chronic autoimmune erythematous-squamous disease that primarily affects the skin, nails, and joints. Psoriasis is known to be a systemic inflammatory condition affecting multiple organs. Patients with psoriasis are at a higher risk of stroke than the general population, and a more severe disease course can increase this risk by up to 44%. One possible explanation for this phenomenon is that chronic systemic inflammation is associated with endothelial dysfunction and atherosclerotic plaque development. On the other hand, patients with psoriasis have an increased prevalence of traditional cardiovascular risk factors, including metabolic syndrome. This narrative review synthesizes the scientific literature to provide a comprehensive overview of the current understanding of the association between psoriasis and AIS.
Introduction
Stroke is the second leading cause of death and disability worldwide (1). In 2020, nearly 12 million people worldwide suffered a stroke, and acute ischemic stroke (AIS) is considered the most common subtype of stroke, accounting for approximately 65% of the total stroke incidence (2). Cheng et al. estimate that the global incidence of stroke will have exceeded 21 million cases by the year 2050 (3). Therefore, primary prevention, which includes not only the management and control of traditional cardiovascular risk factors such as hypertension, diabetes mellitus, dyslipidemia or atrial fibrillation but also lifestyle modifications, should be prioritized in public health (4). Inflammatory and infectious diseases have also long been considered potential risk factors for AIS, but the exact causal relationship remains uncertain (5). Recent studies indicate that autoimmune conditions associated with chronic systemic inflammation are often linked to AIS. Among these, rheumatoid arthritis appears to have the strongest association, yet there is also emerging evidence for the involvement of psoriasis in AIS pathophysiology (6).
Psoriasis is a chronic autoimmune erythematous-squamous disorder defined by proliferative changes predominantly affecting the skin, nails, and joints (psoriatic arthritis) (7–10). The prevalence of psoriasis varies from country to country, e.g., it affects only 0.05% of the general population in Taiwan, which makes it the country with the lowest psoriasis prevalence in the world (11). On the other hand, the prevalence of psoriasis in the United States has been estimated to be as high as 3%, making it one of the most common immune-mediated disorders there (12). Nonetheless, it is a common condition worldwide, affecting people of all ages (7) with a higher prevalence in adults, although it can also occur in children (11). Psoriasis affects both women and men, but in women, the onset typically occurs approximately 10 years earlier than in men, and is more common in patients with a positive family history of the disease (9). The pathophysiology of psoriasis has been linked to genetic susceptibility, in particular the presence of the HLA-C*06:02 risk allele, but also to environmental factors such as tobacco smoking, alcohol consumption, diet, obesity, low physical activity, streptococcal infections or stressful life events (7, 13). However, the exact etiology of psoriasis is complex and remains unclear (14).
For many years, psoriasis was considered a skin disease primarily treated with topical medications and, if necessary, phototherapy. It is now well known that psoriasis is a systemic inflammatory condition with multi-organ involvement (15). This state of chronic low-grade inflammation, usually subclinical, may be associated with comorbidities such as obesity, diabetes mellitus, non-alcoholic fatty liver disease, and cardiovascular disorders (15–17). For instance, according to a systematic review conducted by Correa et al., five out of eight studies included in their analysis indicated that psoriasis increased the risk of myocardial infarction (18). In addition to atherosclerotic diseases, psoriasis might be associated with increased risk of heart failure (19), also in in younger populations (20). According to a cross-sectional study conducted by Eckembrecher et al., among 2,485 hospitalizations of psoriasis patients, 13.7% had comorbid cardiovascular disease (21). Moreover, these individuals tended to have significantly longer hospital stays and generated higher medical costs compared to those without cardiovascular disease (21). Additionally, the risk of developing cardiovascular disorders in psoriatic patients increases with the severity of the underlying disease (17). Notably, the treatment of psoriasis can also modulate the cardiovascular risk profile, with tumor necrosis factor (TNF)-α inhibitors and methotrexate demonstrating beneficial effects (22).
Also, patients with psoriasis are at a higher risk of stroke than the general population, and a more severe course of the disease may increase this risk by 44% (23). A large Danish cohort study based on nationwide registries found that psoriasis is linked to an increased risk of atrial fibrillation (AF), one of the major AIS risk factors in the elderly, as well as to a severity-dependent increase in AIS risk (24). This relationship is complex and not fully understood. Nonetheless, psoriasis is associated with AIS not only through risk factors that are more common in patients with psoriasis but also through shared inflammatory pathways (16, 23). Moreover, endothelial dysfunction might represent a key mechanistic link between chronic systemic inflammation and the elevated cardiovascular risk in patients with psoriasis (25). Finally, in a study by Gelfand et al., the increased risk of stroke was present regardless of the treatment used, whether it potentially increased it, like oral retinoids, or theoretically reduced it, such as methotrexate (26). Figure 1 summarizes the multifaceted connection between psoriasis and AIS.
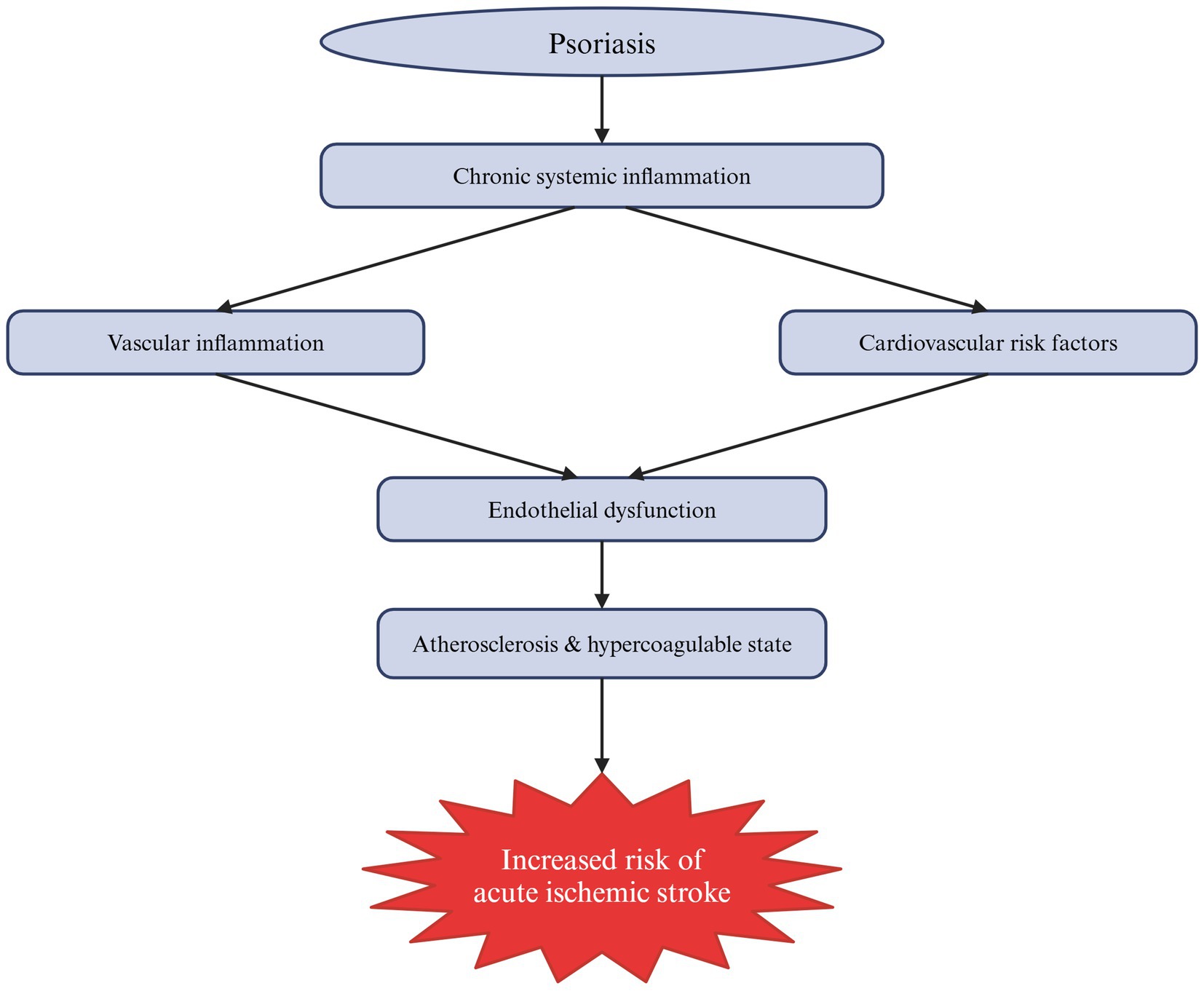
Figure 1. Schematic summary of the mechanisms by which psoriasis contributes to the increased risk of acute ischemic stroke (AIS). As a systemic autoimmune disease, psoriasis is associated with chronic low-grade inflammation that directly affects blood vessels, causing their inflammation, and indirectly influences cardiovascular risk factors. Collectively, these mechanisms lead to endothelial dysfunction, atherosclerosis and a hypercoagulable state, ultimately increasing the risk of AIS.
This narrative review aims to summarize the scientific literature and provide a comprehensive overview of the current understanding of the link between psoriasis and AIS, highlighting the potential role of the inflammatory pathomechanism underlying psoriasis in contributing to AIS incidence. It also explores psoriasis connection to traditional AIS risk factors.
Methodology
A comprehensive literature search was conducted using the PubMed and Google Scholar databases, covering studies from their inception to 5 February 2025. Both experimental and clinical studies were analyzed. A review of the current literature on the relationship between psoriasis and AIS identified key areas to be explored in this review. The pathophysiology of psoriasis and its role in systemic inflammation is discussed, as is the contribution of inflammation as a risk factor for AIS. Also, the analysis extends beyond inflammatory pathways to examine the role of psoriasis-associated comorbidities in stroke development. Titles and abstracts were searched for key terms such as ‘psoriasis’, ‘systemic inflammation’, and ‘acute ischemic stroke’. However, the major limitation of this review is the predominance of observational and cross-sectional studies, which by design, are unable to establish temporal relationships or causality. These studies are prone to a variety of biases, including selection bias. Moreover, the lack of randomized or longitudinal data limits causal inference and underscores the need for more rigorous prospective studies to validate the associations described in this paper. To ensure comprehensive coverage, relevant references from identified articles were also manually reviewed. However, articles written in languages other than English and papers not published as full scientific papers, such as conference abstracts, were excluded from our search to ensure the relevance of the review. The literature search was conducted independently by three authors (PO, KK, RPP) in January and February 2025.
More at link.
 Piotr Olejnik
Piotr Olejnik Kaja Kasarełło
Kaja Kasarełło Renata Podkowińska-Polak3
Renata Podkowińska-Polak3 Aleksandra Golenia
Aleksandra Golenia
No comments:
Post a Comment