Don't follow me but this is what I'm going to do;
Dementia prevention 19 ways
Do not follow my ideas, they are not vetted by any medical team.
http://www.uofmhealth.org/news/archive/201412/mild-memory-and-thinking-issues-what-works-what-doesn%E2%80%99t-u-m
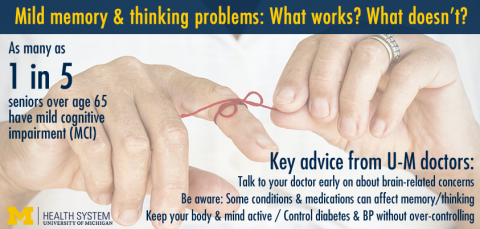
For up to one in five Americans over age 65, getting older brings memory and thinking problems– along with the embarrassment of not being as “sharp” as they once were, and the worry that it will get much worse.
When a senior has mild memory and thinking issues that don't
interfere with daily living, it's called mild cognitive impairment.
What can be done to prevent or slow MCI? And how much should seniors fear that their thinking or memory problems will get much worse? A pair of doctors from the University of Michigan Medical School and VA Ann Arbor Healthcare System have put together a definitive look at the evidence, based on a thorough review of recent studies about MCI.
Published in this week’s issue of the Journal of the American Medical Association, their review article should help doctors and the seniors they treat.
Kenneth Langa, M.D., Ph.D.
“While no medications have been proven to treat MCI successfully,” says Levine, “it’s still a treatable condition. Our review shows good evidence that aerobic exercise, mental activity, social engagement, and stroke prevention help reduce the risk of further cognitive decline.” She notes that the review of medical literature they conducted paid close attention to the quality of the evidence in each study.
Among the key findings of their review, and what they mean for seniors:
- Speak up to your doctor about memory and thinking problems: The new paper offers doctors a step-by-step guide for what to do when a patient or his or her caregiver mentions concerns about memory and thinking problems. Specific lab tests for things like vitamin deficiencies, standard cognitive tests and a full physical and neurological exam can reveal important clues to factors that might be causing their symptoms.
- Keep body and brain active: A number of studies have indicated that aerobic exercise and mental activities can have a small beneficial effect on thinking ability in older adults with MCI.
- Keeping a stroke at bay helps the brain too: Since strokes are brain injuries caused by clots or holes in the blood vessels that keep brain tissue healthy, it makes sense that preventing a stroke can preserve memory and thinking ability. People who have had mini-strokes or survived a full-blown stroke should especially focus on preventing new strokes to keep their brain function as intact as possible as they age, Langa and Levine advise based on the evidence they reviewed. So should people diagnosed with MCI. Having a stroke can worsen cognition and raises the risk of progressing on to dementia.Stroke prevention strategies include controlling high blood pressure, stopping smoking, lowering cholesterol with drugs called statins and taking aspirin or other medicines to prevent blood clots.
- Multiple medicines can fog the brain: Many seniors have prescriptions for a number of medications, and take over-the-counter drugs and supplements, to address their various health risks and conditions. These may have been prescribed or recommended by different doctors – who don’t always know or ask what else a patient is taking. But, say Langa and Levine, studies show that multiple drugs can interact with one another and affect memory and thinking. Doctors and seniors should review all drugs and supplements and see if any interactions can be prevented by reducing the number of medications the patient takes, or stopping drugs that aren’t needed after a hospital stay.
- Avoid over-treatment of high blood pressure and diabetes: While it is important to control blood pressure and diabetes to prevent harmful consequences, doctors need to be careful not to overdo it. “It is important to avoid overtreatment of high blood pressure and diabetes because low blood pressure and low blood sugar may increase the risk of cognitive decline and other patient harms,” says Langa.
- What are the odds?: That’s the key question in the
mind of anyone with suspected or diagnosed MCI – how likely are they to
get worse and progress to dementia and not be able to function
independently. Reassuringly, Levine says, the evidence available shows
that progression from MCI is far from a sure thing.“The numbers are less scary than many people believe,” she notes. “The majority of people with MCI will not progress to dementia and loss of independence, even after 10 years. Some patients with MCI will actually have improved cognition after a year or two, if their cognitive test scores were brought down by an acute illness that gets addressed.” Older adults with MCI are 12 times more likely to die from cardiovascular disease than to die of dementia. So, preventing stroke and heart attack by controlling vascular risk factors is crucial for people diagnosed with MCI.Deborah Levine, M.D., MPH
- More evidence needed for a number of new detection/treatment options: The review of the literature showed that a number of new blood tests and brain imaging options have been proposed and preliminarily tested for diagnosing MCI, and tracking or predicting its progression to dementia. But many of these tests haven’t yet been proven to offer significant benefit to patients, says Langa. And in fact, there can be some risk of “over-diagnosis” when a test identifies a problem that would not go on to cause significant problems for a patient.
Both Langa and Levine are faculty members in the Division of General Medicine at the U-M Medical School, and members of the U-M institute for Healthcare Policy and Innovation and affiliates of the Michigan Alzheimer's Disease Center. Langa also holds positions in the U-M Institute for Social Research and School of Public Health. Levine has a joint appointment in the U-M Department of Neurology. The review article is part of the Care of the Aging Parent series, funded by the SCAN Foundation.
Reference: JAMA, Dec. 17, 2014, Vol. 312 No. 23
No comments:
Post a Comment