FYI. No clue what this says.
A randomized trial of Trendelenburg position for acute moderate ischemic stroke
Nature Communications volume 14, Article number: 2592 (2023)
Abstract
We aim to explore the effect of head-down position (HDP), initiated within 24 hours of onset, in moderate anterior circulation stroke patients with probable large artery atherosclerosis (LAA) etiology. This investigator-initiated, multi-center trial prospective, randomized, open-label, blinded-endpoint, multi-center and phase-2 trial was conducted in China and completed in 2021. Eligible patients were randomly assigned (1:1) into the HDP group receiving −20° Trendelenburg, or control group receiving standard care according to national guideline. The primary endpoint was proportion of modified Rankin Scale (mRS) of 0 to 2 at 90 days, which is a scale for measuring the degree of disability after stroke. 90-day mRS was assessed by a certified staff member who was blinded to group assignment. A total of 96 patients were randomized (47 in HDP group and 49 in control group) and 94 (97.9%) patients were included in the final analysis: 46 in HDP group and 48 in control group. The proportion of favorable outcome was 65.2% (30/46) in the HDP group versus 50.0% (24/48) in the control group (unadjusted: OR 2.05 [95%CI 0.87-4.82], P = 0.099). No severe adverse event was attributed to HDP procedures. This work suggests that the head-down position seems safe and feasible, but does not improve favorable functional outcome in acute moderate stroke patients with LAA. This trial was registered with ClinicalTrials.gov, NCT03744533.
Introduction
To date, there is a paucity of effective neuroprotective treatments for acute ischemic stroke (AIS), other than reperfusion therapy such as intravenous thrombolysis and mechanical thrombectomy, which is limited by a strict therapeutic time window and requirement for a highly developed stroke system of care1. The effect of head position (lying-flat vs sitting-up position) as a nonpharmacological therapy on stroke has been investigated2,3,4,5, but the inconsistent results have led to current ambiguous guideline recommendations1,2,3,4,5,6. It is generally accepted that the supine position may increase blood flow and improve oxygenation2,3,4,7,8,9, but with potential risks such as increased intracranial pressure, cardiopulmonary dysfunction, and aspiration pneumonia10,11,12,13. The neutral results of the Head Positioning in Acute Stroke Trial (HeadPoST) may have been due to the broad inclusion of stroke patients, particularly of patients with milder deficits, which was a key criticism of the trial. While patients with large artery atherosclerosis (LAA) etiology could be a suitable target population14, subgroup analysis of HeadPoST did not detect any evidence of heterogeneity of treatment effect across clinician-diagnosed stroke subtypes15.
In theory, compared with the supine or lying-flat position, the steeper head-down position (i.e., fully supine with Trendelenburg16) could significantly increase blood flow to the ischemic penumbra and improve oxygenation of the brain in the first hours or days after stroke17. Our recent experiment in a rat animal model with middle cerebral artery occlusion showed that the head-down position (HDP) with −30° and 2 h duration after ischemia could improve neurological function and reduce infarct volume18. Moreover, we anecdotally observed several LAA patients in our center, after which a HDP (−20°) averted neurological deterioration and improved clinical outcomes19.
In this work, we undertook the prospective, multicenter, randomized, open-label, blinded-endpoint trial to explore the effect of HDP, initiated within 24 h of symptom onset, in moderate AIS patients with LAA who were not eligible for intravenous thrombolysis or endovascular therapy.
Results
Trial population
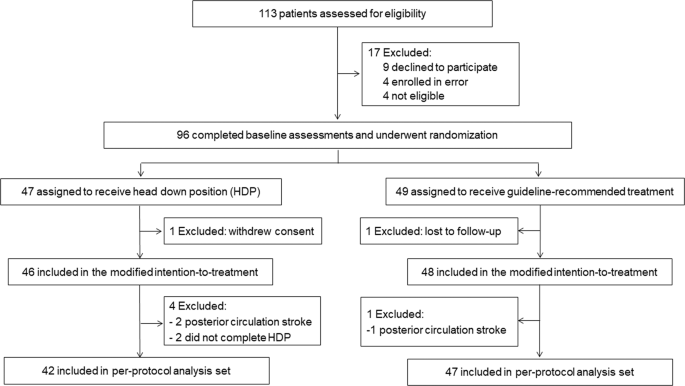
Between Nov 16, 2018, and Aug 28, 2021, 113 consecutive patients were screened and 96 eligible patients were randomly assigned to the HDP group (n = 47) and control group (n = 49). After two patients were excluded, 94 patients were included in the mITT population (46 in the HDP group and 48 in the control group, Fig. 1). The procedure was completed according to the protocol for 89 patients (42 in the HDP group and 47 in the control group), which was included in the per-protocol analysis (Fig. 1). There were no cross-overs between groups in the trial. No patient received carotid or intracranial revascularization. Enrollment was completed in May 2021.
Primary and secondary outcomes
For the primary outcome, the proportion of mRS score 0–2 at 90 days was 65.2% (30/46) in the HDP group and 50.0% (24/48) in the control group (unadjusted OR 2.05 [95% CI 0.87–4.82], p = 0.099; Table 3 and Fig. 2). Similar OR results were observed in the per-protocol analysis (Supplementary Table 2), in the last observation carried forward, worst-case scenario, and best-case scenario sensitivity analyses (Supplementary Table 3), and after adjustment for the prespecified prognostic variables (Table 2).
More at link.
No comments:
Post a Comment