This is where a stroke strategy is needed, not focusing solely on thrombectomy and tPA. By stopping the 5 causes of the neuronal cascade of death in the first week there would be vastly less dead and damaged neurons.
State Policies Might Keep Stroke Patients From the Care They Need

Editor’s note: This story has been updated to remove
information about Hollywood actor Luke Perry being taken by ambulance to
Cedars-Sinai Medical Center after a Feb. 27 stroke. Contrary to local
news reports, a representative of the hospital stated that the actor was
not taken there.
More than 140,000 Americans die from stroke every year. But getting to the best hospital as quickly as possible after a stroke improves your chances of survival. And where an ambulance takes you could depend on state law.
Unlike state rules for accident victims, which uniformly require first responders to take severely injured patients to the most advanced trauma unit available, state policies for stroke patients vary widely.
Most state rules direct paramedics to the closest hospital with a stroke unit, regardless of the attack’s severity. And some states limit paramedics to taking stroke patients to hospitals within state borders.
But most of those rules came before the recent advent of thrombectomy surgery to remove blood clots from the brain. New research shows the procedure gives patients who suffer a severe stroke a much better chance of survival without impairments.
As a result, about half of states are working to change their EMS rules and policies to ensure the most-critical patients get the surgery as quickly as possible. Neurological professional groups recommend that if a comprehensive stroke unit is within a two-hour flight or drive, then severe stroke patients should be transported there, even if a lower-level stroke unit is closer.
More than 140,000 Americans die from stroke every year. But getting to the best hospital as quickly as possible after a stroke improves your chances of survival. And where an ambulance takes you could depend on state law.
Unlike state rules for accident victims, which uniformly require first responders to take severely injured patients to the most advanced trauma unit available, state policies for stroke patients vary widely.
Most state rules direct paramedics to the closest hospital with a stroke unit, regardless of the attack’s severity. And some states limit paramedics to taking stroke patients to hospitals within state borders.
But most of those rules came before the recent advent of thrombectomy surgery to remove blood clots from the brain. New research shows the procedure gives patients who suffer a severe stroke a much better chance of survival without impairments.
As a result, about half of states are working to change their EMS rules and policies to ensure the most-critical patients get the surgery as quickly as possible. Neurological professional groups recommend that if a comprehensive stroke unit is within a two-hour flight or drive, then severe stroke patients should be transported there, even if a lower-level stroke unit is closer.
In January, Ohio joined Arizona, Colorado, Rhode Island, Tennessee and Virginia in requiring paramedics to take patients with a severe stroke directly to a hospital with a comprehensive stroke center that has been licensed to perform thrombectomies, provided it’s possible to reach one within a specified amount of time.
Florida, Massachusetts and New York are close to adopting similar updates to their emergency stroke policies this year.
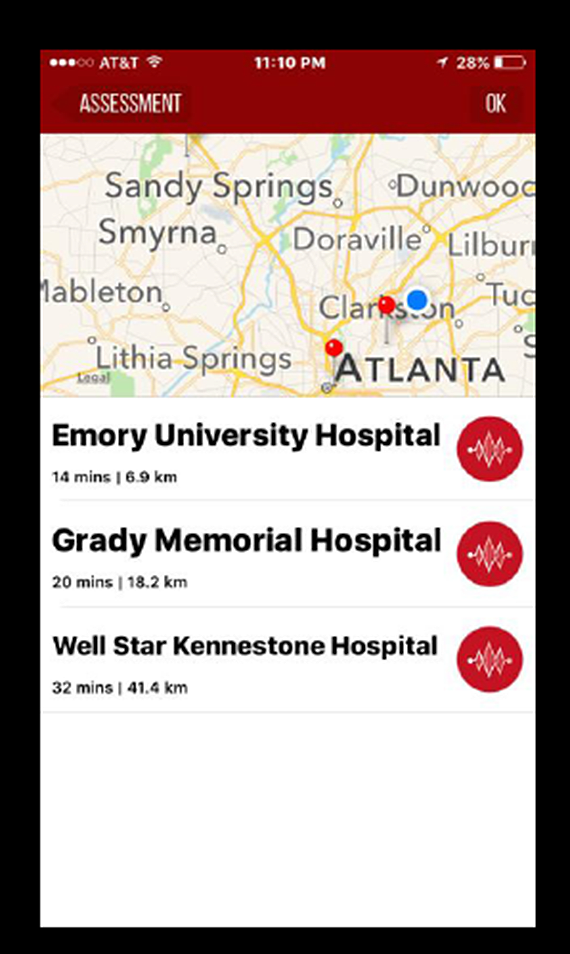
Statewide mandatory stroke protocols don’t require paramedics in Florida, Georgia, Indiana and Oklahoma to transport severe stroke patients directly to a hospital that can perform thrombectomies. But some paramedics in those states are using a free smartphone app called Fast-ED to screen stroke patients for severity, locate a comprehensive stroke unit, notify the unit, and drive there as quickly as possible.
Other local and regional cooperative efforts among hospitals and paramedics are helping ensure that patients are transported to the most appropriate hospital. But nationwide, emergency stroke protocols are a jumble.
“In any state in the country, if a person is shot, first responders know where the trauma unit is. They’ll bypass a little community hospital and go straight to the trauma center. The same thing needs to happen for stroke victims,” said Dr. Adam Arthur, a neurosurgeon at the Semmes Murphey Clinic in Memphis, Tennessee.
Still, not everyone agrees that getting more patients to comprehensive stroke centers is the most critical issue in preventing stroke fatalities.
U.S. Centers for Disease Control and Prevention stroke expert Dr. Sallyann Coleman King said it wouldn’t be practical to take every patient to a comprehensive stroke center. “Even if we had all the money and resources needed to make all centers a comprehensive stroke center,” she said, “it just wouldn’t make sense.”
First, the public needs to know to call 911 if someone is having a stroke, she said.
About half of all stroke patients arrive at a hospital by other means than an ambulance. They get a ride from a friend or neighbor, or they take a taxi. “We’re trying to get the word out that stroke care starts in the ambulance,” King said.
“What makes sense is creating a system of care where the community and patients know the signs and symptoms of stroke and to call 911,” she said. “The EMS system is prepared to gather the needed information, assess the patient, and take them to the appropriate facility to best treat their stroke.”
Growing Evidence
The need for new emergency stroke protocols sprang largely from the results of recent clinical trials showing that thrombectomies are highly effective at preventing stroke fatalities and limiting disabilities.In 2004, the U.S. Food and Drug Administration approved the first device for manual thrombectomy surgery — in which a catheter is inserted into an artery in the groin and threaded up through the neck until it reaches an arterial blood clot in the brain. Then the artery is expanded and the clot is grabbed by a special device at the end of the catheter and removed.
It took 11 years to improve the device design and ultimately prove the surgery’s effectiveness at treating stroke.
By 2015, the surgery had been performed on thousands of patients, and catheters and instruments designed to remove arterial clots had improved. More recently, two landmark clinical trials — one in Germany and one in the Netherlands — proved its effectiveness for wider use.
Increasingly, paramedics and emergency physicians began realizing that thrombectomy surgery could be more important for patients with blood clots in large brain arteries than lower levels of treatment, such as clot-busting medications that, in many cases, could be administered more quickly.
A 2018 study conducted by researchers at Grady Memorial Hospital in Atlanta and the University of Pittsburgh Medical Center showed that severe stroke patients who received a thrombectomy within 24 hours of a stroke survived without disabling brain damage at a much higher rate than those who received only traditional treatments.
Until recently, however, nearly all first responders were taking stroke patients to the closest hospital, where emergency physicians typically would decide whether to transfer patients by ground or air to a comprehensive stroke unit for a thrombectomy.
A study published in January by Duke University researchers showed that patients who were taken directly to a hospital capable of performing a thrombectomy had better outcomes(but we expect 100% recovery. What are you doing to get there?) than those who were first transported to a local hospital and later transferred to a comprehensive stroke center.
A dose of clot-busting medicine costs more than $6,000. Mechanical thrombectomy costs about twice as much.
Stroke Mortality Rates in 2017
Stroke death rate per 100,000 total population
37.6
U.S. age-adjusted rate of stroke death
Show Data Table
The rate of stroke deaths varies widely among states. Some states
are enacting laws and policies to improve the chances of survival for
stroke victims by ensuring that emergency medical services take patients
to the closest and most appropriate stroke emergency center available.
Source: U.S. Centers for Disease Control and Prevention, “Stroke Mortality by State”
Source: U.S. Centers for Disease Control and Prevention, “Stroke Mortality by State”
Copyright © 1996-2019 The Pew Charitable Trusts. All rights reserved.
The vast majority of strokes, nearly 800,000 a year in the United States, are ischemic strokes involving a blood clot in an artery in the brain. Of those, about 11 percent are severe, involving clots in large arteries that cut off a substantial amount of blood flow. Those patients could benefit from a thrombectomy.
But fewer than 10 percent of eligible patients receive the surgery, according to the Society of NeuroInterventional Surgery, an international scientific organization that advocates for greater public access to thrombectomies.
In 2018, in a set of guidelines on emergency procedures for stroke victims, the American Heart Association wrote: “When several [stroke] capable hospital options exist within a defined geographic region, the benefit of bypassing the closest to bring the patient to one that offers a higher level of stroke care, including mechanical thrombectomy, is uncertain. Further research is needed.”
But after an outcry from neurosurgeons familiar with the procedure and the research behind it, the organization retracted the guidelines. A representative of the American Heart Association wrote in an email to Stateline that the organization is working on an update.
Improving Survival(With no strategy you can't fix the problems in stroke)
Stroke and related heart disease are the leading cause of death in the world, accounting for a combined 15.2 million deaths in 2016, according to the World Health Organization.The fifth-leading cause of death in the United States, strokes also are a major cause of adult disability. The condition, sometimes called a “brain attack,” occurs every 40 seconds, according to the CDC.
Thanks to improved diets, increased physical activity and reduced smoking, the incidence of strokes has been declining in the United States since the 1970s, according to a statement by the American Heart Association. At the same time, survival rates have been rising.
But among patients who survive a major stroke, about 40 percent have impairments that require specialized care, sometimes for life. Age and the severity of a stroke are major determinants of how a person will fare following a stroke.
According to the Society of NeuroInterventional Surgery, 65 percent of patients taken directly to a comprehensive stroke center survive without long-term disabilities, compared with 42 percent of people taken to the nearest hospital with a less-advanced stroke center.
Advocates predict that as more hospitals develop the expertise to perform thrombectomies, and as more patients get access to the surgery, disability-free survival rates for stroke victims will rise even higher.


No comments:
Post a Comment