You'll need your incompetent doctors and hospital to step up and ensure human testing gets done! But that won't occur, will it?
Stroke breakthrough takes aim at the gut
What does gut fermentation and stroke-induced brain inflammation have in common? Potentially a lot, according to new research looking into how the microbiome directly influences brain inflammation. It could make recovery faster, reduce cognitive impairment and protect the brain from secondary injuries following a stroke.
Scientists from The University of Texas Health Science Center at Houston (UTHealth Houston) have turned their attention to the gut – in particular, the ligands produced there. Ligands, produced in the gut as well as elsewhere in the body, are important molecules that bind to specific receptors – proteins on the surface of a cell – and play a crucial role in signaling and cell function. Some of these ligands serve as neurotransmitters and are essential for healthy neuronal activity.
The researchers were particularly interested in the gut-produced ligands that bind to the aryl hydrocarbon receptor (AhR) – AHR ligands – which impact immune response and inflammation in the body – including in the brain. Following a stroke, the gut's microbiota is compromised, resulting in an imbalance (dysbiosis) which in turn leads to a drop in gut-produced AHR ligands (dysbiosis). At the same time, there's an uptick in Kynuerine (Kyn) AHR ligands, not derived from the gut, and their overactivity results in neuroinflammation dysregulation. Ultimately, without the gut-sourced ligands binding to receptors of the microglia – the central nervous system's immune cells – in the brain, the imbalance can leave post-stroke neuroinflammation difficult to reduce, potentially leading to secondary brain injury and damage.
As such, the gut-derived ligands are essential in regulating and reducing inflammation. It's further evidence of the relationship between the gut and brain, particularly when it comes to inflammation. Late last year, research out of another Texan institute, Texas A&M University, also found that post-stroke gut health had a direct impact on the brain and recovery.
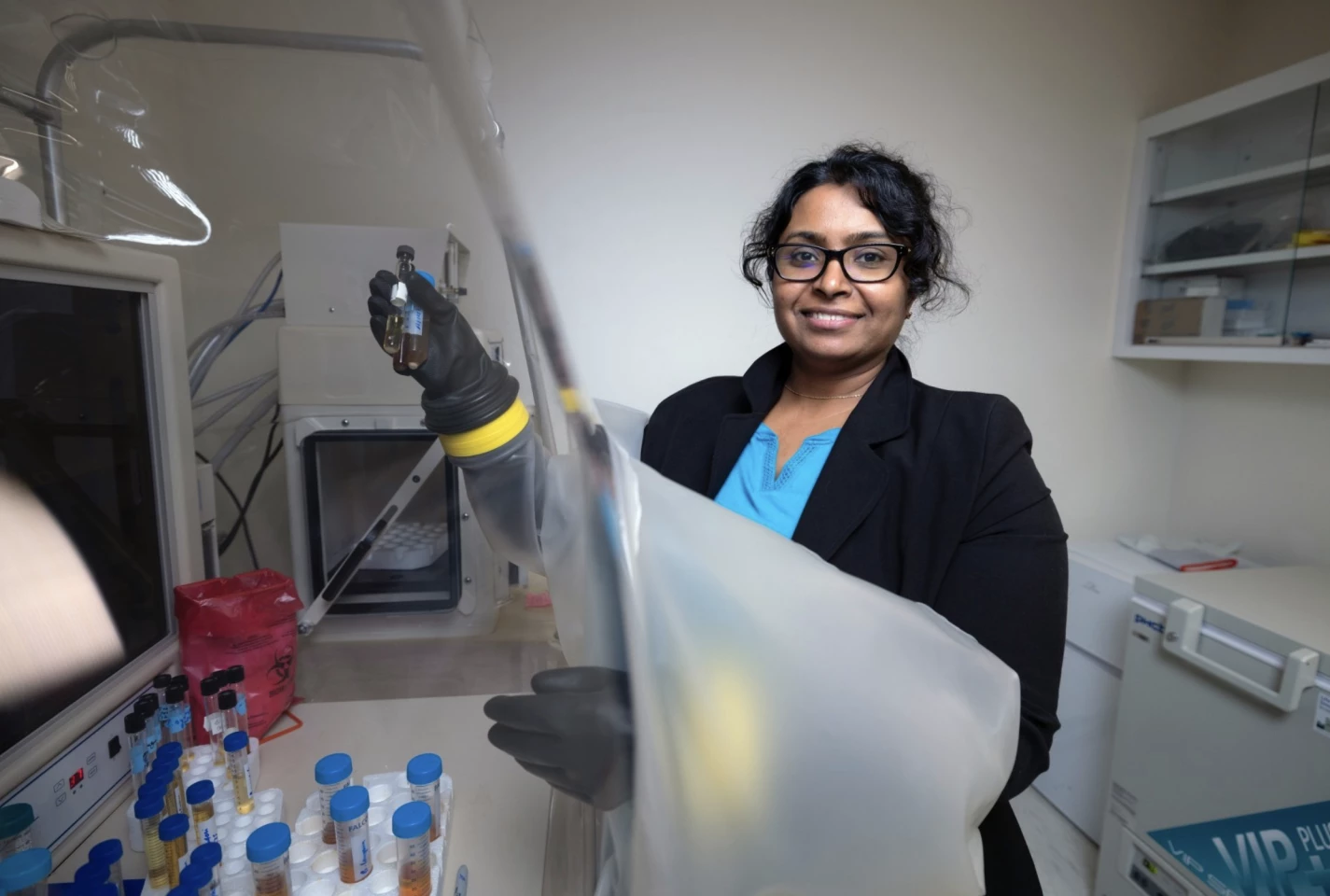
“This study looked at how substances from the body and gut bacteria called AHR ligands affect post-stroke inflammation,” said senior author Bhanu Priya Ganesh, associate professor of neurology with McGovern Medical School at UTHealth Houston. “They found that after a stroke, changes in gut bacteria lead to a drop in beneficial substances and an increase in harmful ones. This suggests that restoring these beneficial substances from gut bacteria could help reduce inflammation after a stroke.”
In an earlier preclinical animal study, the researchers showed how stroke and other neurodegenerative diseases disrupt the gut microbiota, which in turn affects brain function – and that dysbiosis worsened with age. It again underpinned the critical role of the microbiota-gut-brain-axis (MGBA).
Now, once again studying aged mice, the team has demonstrated how restoring the gut's balance following a stroke, in order to provide the right fermentation environment for those important ligand metabolites to be made, can ultimately reduce neuroinflammation.
“Our recent animal-model study points to new treatment options that could focus on the gut-brain connection, offering potential ways to improve recovery after a stroke and reduce brain damage,” Ganesh said.
While the team identified some limitations, such as a sex difference in beneficial outcomes (their research focused on aged male mice, which had the strongest cognitive response), it's nonetheless an important discovery into improving brain function and recovery for stroke patients.
"Restoring a balanced pool of host- and microbiota-derived AHR ligands may be beneficial after stroke and may represent a therapeutic target," the researchers wrote.
The study was published in the journal Nature Communications.
Source: UTHealth Houston
No comments:
Post a Comment