Nothing here told me anything useful in understandable actions I could take even though this was in TBI not stroke.
Rebuilding Microbiome for Mitigating Traumatic Brain Injury: Importance of Restructuring the Gut-Microbiome-Brain Axis
Molecular Neurobiology (2021)
Abstract
Traumatic brain injury (TBI) is a damage to the brain from an external force that results in temporary or permanent impairment in brain functions. Unfortunately, not many treatment options are available to TBI patients. Therefore, knowledge of the complex interplay between gut microbiome (GM) and brain health may shed novel insights as it is a rapidly expanding field of research around the world. Recent studies show that GM plays important roles in shaping neurogenerative processes such as blood-brain-barrier (BBB), myelination, neurogenesis, and microglial maturation. In addition, GM is also known to modulate many aspects of neurological behavior and cognition; however, not much is known about the role of GM in brain injuries. Since GM has been shown to improve cellular and molecular functions via mitigating TBI-induced pathologies such as BBB permeability, neuroinflammation, astroglia activation, and mitochondrial dysfunction, herein we discuss how a dysbiotic gut environment, which in fact, contributes to central nervous system (CNS) disorders during brain injury and how to potentially ward off these harmful effects. We further opine that a better understanding of GM-brain (GMB) axis could help assist in designing better treatment and management strategies in future for the patients who are faced with limited options.
Introduction
Traumatic brain injury (TBI) occurs due to an external force causing skull damage which could invariably affect the brain [1]. The trauma leading to brain injury can be broadly categorized as an impact or a non-impact event depending upon whether the external object had a direct contact with the head (impact) or was it a non-impact force like the blast waves or a rapid acceleration, and deceleration (non-impact) with the head [2]. In the USA, frequency of TBI occurs every 15 s (roughly about 1.7 million new TBI cases/year) and costs more than US $77 billion/year [3]. In brief, TBI events are responsible for 50,000 deaths together with 80,000 individuals that are left with permanent disabilities each year [4,5,6,7]. It is believed that the frequency of brain injury is estimated to be higher than any other type of diseases such as Parkinson’s disease, multiple sclerosis, AIDS, and breast carcinoma [3]. For example, motor-vehicle or traffic-related accidents constitute 17% cases while walking-falls are responsible for 35% of cases in USA [4,5,6,7]. As per one estimate 130,000 children in the age between 5 and 18 years suffered from sport-related concussions [8]. Besides, blast injury was the most common cause of TBI-related event that was observed among the military personnel [9]. In recent years, several experimental animal models have been developed to replicate human TBI pathophysiological aspects employing the pre-clinical settings [10] including fluid percussion, weight-drop injury, and controlled cortical impact (CCI). These animal models are routinely used in simulating TBI-related events in small animals with characteristics of mild or severe TBI. In fact, these models remain the workhorses for studying characteristic features of the primary, as well as secondary brain injuries in humans [11].
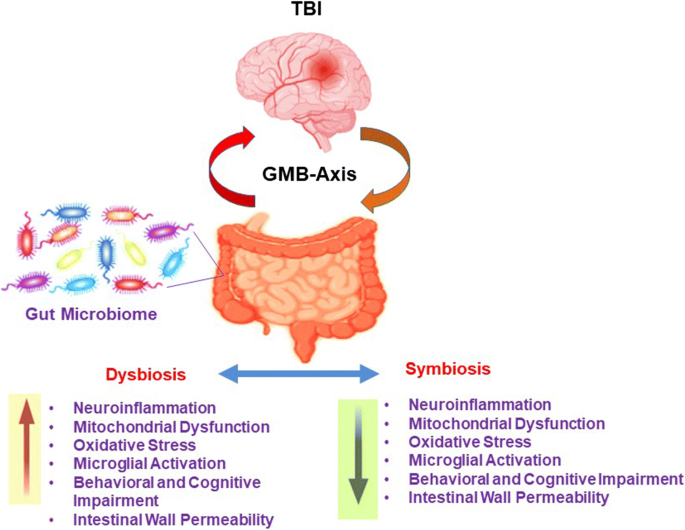
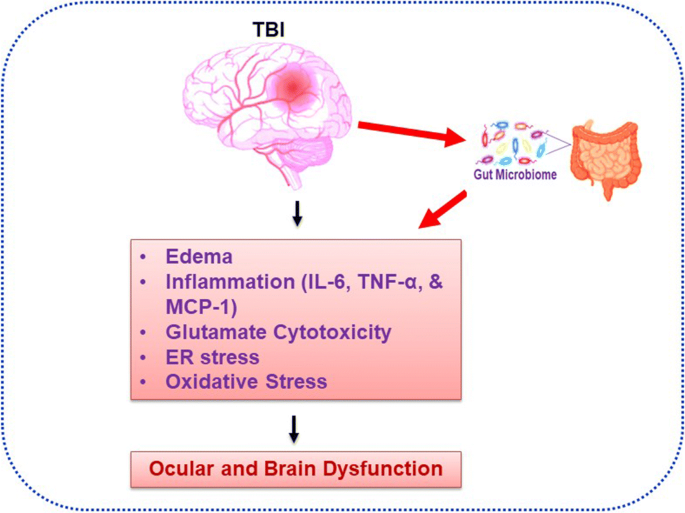
An acquired insult during TBI could potentially change various structural components of the brain resulting in temporary or even permanent brain impairment [12, 13]. Interestingly, GM and its role(s) in various system disorders has recently been the major focus area of research worldwide. For example, previous work reveals that GM plays important roles in neurogenerative processes such as formation of BBB, myelination, neurogenesis, and microglial maturation [14]. It has been shown that microbiome also modulates many aspects of our behavior since GM is involved in the modulation of cellular and molecular processes by balancing microbial eubiosis and dysbiosis condition and also involved in the progression of TBI-induced pathologies including BBB permeability, immune response to neuroinflammation, astroglial activation, and mitochondrial dysfunction (Fig. 1) [14]. Currently, efficacious treatments for TBI patients are acutely lacking [15,16,17]. Additionally, gut dysbiosis is known to exacerbate behavioral impairment as shown in studies that employed animal models of TBI and the spinal cord injury [18,19,20,21]. Furthermore, the dysbiotic milieu negatively affects the post stroke recovery [22,23,24,25]. Treatments for TBI and related disorders are severely limited, but recent research shows that microbiome transplants could mitigate CNS damage and functional impairments in spinal cord injury and stroke in animals [18]. In addition, probiotics were shown to reduce the rate of infections and time spent in intensive care units of hospitalized patients suffering from the brain trauma [18, 26, 27]. Thus, establishment of a protective, that is, eubiotic GM, is a promising therapeutic avenue since the brain injuries induce dysbiosis (Fig. 2). Reiner and colleagues 2014 reported that Novel CB2 Inverse Agonist SMM-189 reduce motor, visual, and emotional deficits after closed-head mild traumatic brain injury mouse model via mitigation of microglial inflammatory action [28]. ER stress was found to be increased early in juvenile rats exposed to TBI and that these rats developed tau oligomers over the course of 30 days and had significant short-term and spatial memory deficits following injury [29]. Treangen and colleagues suggested that acute bacterial dysbiosis within the gut microbiome was observed after TBI post-injury in mice [30]. The overall researched layout is represented in Fig. 2. However, post-TBI associated ocular and brain dysfunction via direct regulation of altered gut microbiome homeostasis is still needed to be demonstrated. This review discusses how GM alterations during post TBI contribute to CNS dysfunction and how to potentially target GM for therapeutic benefits in patients.
TBI induced dysbiosis via the gut microbiome brain (GMB) axis. The GMB-axis could potentially contribute, and further worsen the injury profile by promoting dysbiosis over eubiosis wherein harmful microbes in the gut can lead to an increase in neuroinflammation, mitochondrial dysfunction, oxidative stress, microglial activation, behavioral, and cognitive impairment, and intestinal wall permeability.



 Auwal Abdullahi
Auwal Abdullahi Steven Truijen2,
Steven Truijen2,  Ushotanefe Useh
Ushotanefe Useh Tamaya Van Criekinge
Tamaya Van Criekinge