ABSOLUTELY USELESS. Nothing here helps any survivor recover better.
Relationship between gait quality measures and modular neuromuscular control parameters in chronic post-stroke individuals
Journal of NeuroEngineering and Rehabilitation volume 18, Article number: 58 (2021)
Abstract
Background
Recent evidence suggests that disinhibition and/or hyperexcitation of the brainstem descending pathways and intraspinal motor network diffuse spastic synergistic activation patterns after stroke. This results in simplified or merged muscle sets (i.e., muscle modules or synergies) compared to non-impaired individuals and this leads to poor walking performance. However, the relations of how these neuromuscular deficits influence gait quality (e.g., symmetry or natural walking patterns) are still unclear. The objective of this exploratory study was to investigate the relations of modular neuromuscular framework and gait quality measures in chronic stroke individuals.
Methods
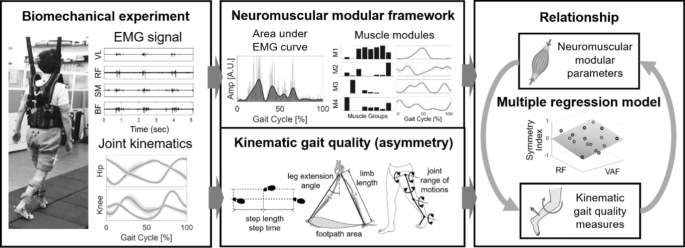
Sixteen chronic post-stroke individuals participated in this study. Full lower body three-dimensional kinematics and electromyography (EMG) were concurrently measured during overground walking at a comfortable speed. We first examined changes in gait quality measures across the number of muscle modules using linear regression model. Then, a stepwise multiple regression was used to investigate the optimal combination of the neuromuscular parameters that associates with gait quality measures.
Results
We observed that subjects who had a lower number of muscle modules revealed reduced function (i.e., speed) and greater asymmetry in the kinematic parameters including limb length, footpath area, knee flexion/extension, and hip abduction/adduction (all p < 0.05). We also found that the combination of input variables from the modular neuromuscular control framework significantly associated with gait quality measures (average R2=42.5%). Those variables included variability accounted for (VAF) information from the muscle modules and area under the EMG envelope curves of the quadriceps (i.e., rectus femoris and vastus lateralis) and tibialis anterior muscles.
Conclusions
The results suggest that there exists a significant correlation between the neuromuscular control framework and the gait quality measures. This study helps to understand the underlying mechanism of disturbances in gait quality and provides insight for a more comprehensive outcome measure to assess gait impairment after stroke.
Background
Effective gait recovery after a stroke involves improvements both in functional mobility and quality of movement. However, conventional clinical outcomes measuring gait such as Ten Meter Walk Test (10MWT), Six Minute Walk Test (6MWT), and Timed-Up-and-Go (TUG) focus on functional indices that provide a holistic picture of walking performance and recovery [1,2,3]. On the other hand, an increased number of recent studies accentuate the importance of monitoring detailed gait quality to assess gait impairments [4]. Disturbances in gait quality are associated with an increased risk of falls [5], greater energy expenditure [6], and long-term problems such as learned non-use or use-dependent plasticity, musculoskeletal injuries, and pain [7, 8].
Symmetry is a common measure to characterize disturbances in gait quality. While spatiotemporal symmetry (e.g., step length, step time) has been well charted to describe gait after stroke [9], kinematics would arguably be the most detailed way to represent the human movements including gait after stroke. Post-stroke individuals exhibit significant asymmetry in joint kinematics with greater inter-individual variability than spatiotemporal measures [10]. Typical asymmetry in joint kinematics includes reduced hip extension, knee flexion and ankle dorsi/plantar flexion, and knee hyperextension on the impaired side [11]. Limb kinematics, related to the end-effector (i.e., foot) motion in task space, has also been indicated as an important parameter for locomotor function [4]. For instance, Shin et al., found that post-stroke individuals preferentially coordinated the paretic side of limb function using limb kinematics by compensating joint kinematics during walking [4].
Neuromuscular activity is crucial to execute biomechanical functions such as gait [12]. Previous studies have shown that muscle activity during walking can be grouped into sets of co-excited muscles (also known as muscle modules or synergies) [13]. While there is an ongoing debate on whether these modules are originated from neural plasticity shaped by repetitive activities or encoded in central nervous system, a general consensus is that modules may reduce the computational cost in selecting strategies of motor coordination [14, 15]. Previous studies have identified that well-coordinated gait in healthy individuals can be produced by a small number between four to five group of modules [13, 16]. Other studies suggest that the concept of muscle modules can be used as an outcome measure to assess motor recovery following therapeutic interventions [17].
Recent evidence suggests that disinhibition and/or hyperexcitation of the brainstem descending pathways and intraspinal motor network diffuse spastic synergistic activation post-stroke [18]. As a result, simplified or merged muscle modules compared to non-impaired individuals are typically observed and lead to poor walking performance, for instance, reduced walking speed with greater spatiotemporal asymmetry than those of healthy individuals [13]. Several other previous studies discussed the impact of neuromuscular deficit on gait impairments or deviations after stroke [19, 20]. For example, Barroso et al. combined biomechanics and modular parameters to predict measures of walking asymmetry such as paretic limb propulsion or paretic stride ratio [20]. While these studies may provide multifaceted picture of walking performance and recovery, an additional endeavor to find how detailed kinematic gait quality measures are influenced by neuromuscular deficits, such as merged muscle modules, may help to better delineate the underlying causality among impairments and locomotor functions after stroke.
The objective of this exploratory study was to investigate the relations of modular neuromuscular deficits and disturbances in gait quality measures (i.e., asymmetry) in terms of spatiotemporal, limb and joint kinematic parameters in chronic post-stroke individuals (see Fig. 1). We measured lower body electromyography (EMG) activities and gait kinematics concurrently during walking from 16 chronic post-stroke participants. We hypothesized that the post-stroke individuals with a reduced number of muscle modules will exhibit greater asymmetry in gait quality measures due to the loss of independence in motor activations [13]. Accordingly, we also expected to find a strong association between the gait quality measures and the input modular neuromuscular control framework assuming a causal relationship exists in these measures [21].
No comments:
Post a Comment