Oh, a new big word that I guess is supposed to impress us:
exoneuromusculoskeleton
Home-based self-help telerehabilitation of the upper limb assisted by an electromyography-driven wrist/hand exoneuromusculoskeleton after stroke
Journal of NeuroEngineering and Rehabilitation volume 18, Article number: 137 (2021)
Abstract
Background
Most stroke survivors have sustained upper limb impairment in their distal joints. An electromyography (EMG)-driven wrist/hand exoneuromusculoskeleton (WH-ENMS) was developed previously. The present study investigated the feasibility of a home-based self-help telerehabilitation program assisted by the aforementioned EMG-driven WH-ENMS and its rehabilitation effects after stroke.
Methods
Persons with chronic stroke (n = 11) were recruited in a single-group trial. The training progress, including the training frequency and duration, was telemonitored. The clinical outcomes were evaluated using the Fugl–Meyer Assessment (FMA), Action Research Arm Test (ARAT), Wolf Motor Function Test (WMFT), Motor Functional Independence Measure (FIM), and Modified Ashworth Scale (MAS). Improvement in muscle coordination was investigated in terms of the EMG activation level and the Co-contraction Index (CI) of the target muscles, including the abductor pollicis brevis (APB), flexor carpi radialis-flexor digitorum (FCR-FD), extensor carpi ulnaris-extensor digitorum (ECU-ED), biceps brachii (BIC), and triceps brachii (TRI). The movement smoothness and compensatory trunk movement were evaluated in terms of the following two kinematic parameters: number of movement units (NMUs) and maximal trunk displacement (MTD). The above evaluations were conducted before and after the training.
Results
All of the participants completed the home-based program with an intensity of 63.0 ± 1.90 (mean ± SD) min/session and 3.73 ± 0.75 (mean ± SD) sessions/week. After the training, motor improvements in the entire upper limb were found, as indicated by the significant improvements (P < 0.05) in the FMA, ARAT, WMFT, and MAS; significant decreases (P < 0.05) in the EMG activation levels of the APB and FCR-FD; significant decreases (P < 0.05) in the CI of the ECU–ED/FCR–FD, ECU–ED/BIC, FCR–FD/APB, FCR–FD/BIC, FCR–FD/TRI, APB/BIC and BIC/TRI muscle pairs; and significant reductions (P < 0.05) in the NMUs and MTD.
Conclusions
The results suggested that the home-based self-help telerehabilitation program assisted by EMG-driven WH-ENMS is feasible and effective for improving the motor function of the paretic upper limb after stroke.
Trial registration ClinicalTrials.gov. NCT03752775; Date of registration: November 20, 2018.
Introduction
Most patients with stroke who are discharged home from inpatient poststroke rehabilitation have residual motor impairment of the upper limb, especially in the distal joints (i.e., the wrist and the fingers), which greatly inhibits their ability to perform activities of daily living (ADLs) [1, 2]. Although the traditional viewpoint on poststroke rehabilitation suggested that significant motor recovery mainly occurs in the first 6 months after the onset of a stroke (i.e., acute and subacute periods) [3], more recent studies have indicated that significant motor improvements could also be achieved in the chronic period after stroke through physical training as long as such training is as intensive as the one provided to inpatients [4, 5]. Continuous and regular physical therapy is required to improve the wrist/hand function of outpatients with chronic stroke [6]. The restoration of limb function after stroke depends on intensive and repetitive training of the paralyzed limb [7, 8] with maximized voluntary motor effort [9, 10] and minimized compensatory motions in close-to-normal muscular coordination [10, 11]. However, the provision of effective wrist/hand rehabilitation services for outpatients with chronic stroke is insufficient in the current healthcare system in the world.
In most cases, outpatients have limited access to wrist/hand treatments with the necessary training intensity [12, 13] because of resource constraints due to factors such as an expanding stroke population and a lack of professionals worldwide [14, 15], as well as other difficulties such as commuting [2] to the outpatient services in day hospitals, and the restriction of social distancing during the COVID-19 pandemic. Home-based telerehabilitation with minimum assistance and remote supervision by professionals (i.e., self-help operation) is a promising approach for sustaining of physical treatment after discharge and enhancing the accessibility of rehabilitation resources to improve the wrist/hand motor functions of discharged patients [16,17,18].
However, few studies have focused on techniques for effective self-help upper limb rehabilitation, especially for distal joints [16]. Currently, most studies on home-based telerehabilitation have been based on virtual reality (VR) techniques because home-based VR training is more convenient for and accessible to outpatients than conventional therapy in a clinic or day hospital [16, 19]. Nevertheless, those systems focus on assessment or monitoring of limb performance rather than providing the necessary physical assistance for the patients to achieve the desired movements [16, 20,21,22,23,24]. Rehabilitation robots have been developed to provide mechanical assistance that mimics physical support from a therapist in conventional therapy; these robots can alleviate the labor-intensive aspects of hands-on physical therapy by performing repetitive therapeutic tasks intensively under the supervision of a therapist [15], and these robotic therapies for distal joints have been reported to be effective for improving upper limb motor function [1, 25]. However, the majority of the existing rehabilitation robots are heavy, have complex mechanical designs, and require large power supplies, large physical spaces in conventional environments (e.g., clinic), and close professional supervision, which are significant deterrents to their use by patients independently at home [15, 26].
Furthermore, using robot alone has a limitation in directly activating the desired muscle groups because the target muscles of patients with stroke usually cooperate with compensatory motions from other muscular activities [27]. Compensatory motions from the trunk and the proximal joints, i.e., abnormal motor synergies, are commonly observed in most persons with chronic stroke when they attempt to reach an object or orient their hand to grasp an object [28]. When neuromuscular electrical stimulation (NMES) combined with robotic therapy, the robotic assistance could provide sensorimotor experiences with precise kinematics to realize the desired movements [29], and NMES could activate the target muscles and reduce compensation from alternative muscle synergies [30]. Thus, the combined NMES-robot treatment has been suggested to facilitate close-to-normal muscular coordination with reduced compensation motions, and it has yielded more effective rehabilitation outcomes than upper limb rehabilitation treatments that use only NMES or only robots [31]. Electromyography (EMG) of the paralyzed limb to indicate voluntary intention to integrate voluntary motor effort during practice has been recommended for optimizing therapeutic outcomes [32]. EMG-driven training systems have yielded superior improvements in motor functions with longer sustainability than those with passive limb motions [33], especially for voluntary motor control of the upper limb. Therefore, EMG-driven NMES-robot therapy for home-based self-help training is desirable for effective wrist/hand rehabilitation for outpatients with chronic stroke.
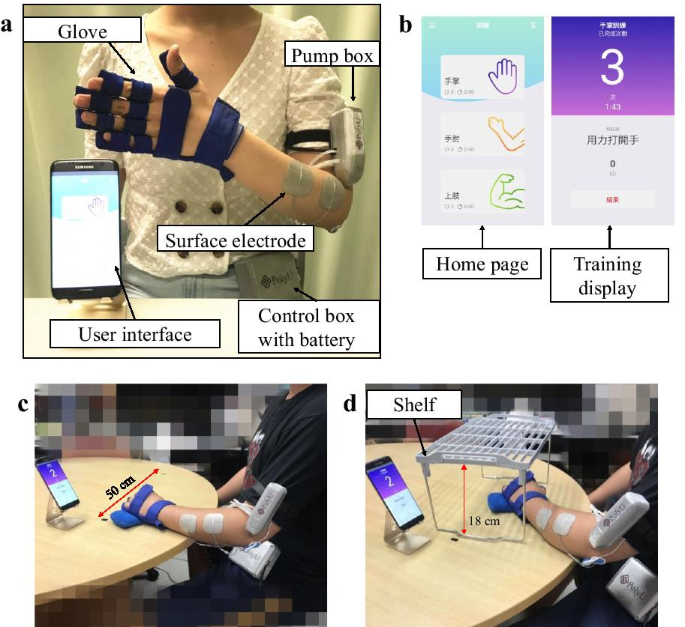
A novel EMG-driven exoneuromusculoskeleton (ENMS) for self-help upper limb rehabilitation after stroke was developed recently by our team [34, 35]. Taking the advantages of exoskeleton, pneumatic muscle, and NMES, the developed system is lightweight, compact, and has low power consumption. The system can assist the extension and flexion of the elbow, wrist, and finger joints under voluntary effort control through EMG. The system consists of an elbow module and a wrist/hand module that can work collectively or separately. The wrist/hand module can work independently as an EMG-driven wrist/hand ENMS (WH-ENMS) to assist wrist/hand movements during training (Fig. 1). The rehabilitation effects of the EMG-driven ENMS have been investigated in 15 participants with chronic stroke [35], followed by a 20-session training program in a neurorehabilitation laboratory, where the participants completed the training independently with the system after they received a tutorial session and three guided training sessions (including practicing device operation and training setup). The participants exhibited significant improvements in voluntary motor control and muscle coordination of the paretic limb after the EMG-driven ENMS-assisted upper limb training [35]. No safety problems were reported by either the experiment operators or the participants throughout the study period. The system offers the possibility of home-based self-help wrist/hand training for discharged patients with chronic stroke. However, the feasibility of using the EMG-driven WH-ENMS for self-help upper limb training and its rehabilitation effects in a home setting had not been investigated.
Therefore, in this study, we aimed to determine the feasibility of home-based self-help training assisted by the EMG-driven WH-ENMS on outpatients with chronic stroke and investigate its rehabilitation effects. Our hypothesis was that the participants who received the home-based self-help telerehabilitation training assisted by the EMG-driven WH-ENMS would obtain motor improvements in the distal joints, better muscle coordination of the paretic upper limb, and reduce compensatory movements when performing limb tasks.
No comments:
Post a Comment