I don't see the Regent suit from Russia.
Human-centered design of a novel soft exosuit for post-stroke gait rehabilitation
Journal of NeuroEngineering and Rehabilitation volume 21, Article number: 62 (2024)
Abstract
Background
Stroke remains a major cause of long-term adult disability in the United States, necessitating the need for effective rehabilitation strategies for post-stroke gait impairments. Despite advancements in post-stroke care, existing rehabilitation often falls short, prompting the development of devices like robots and exoskeletons. However, these technologies often lack crucial input from end-users, such as clinicians, patients, and caregivers, hindering their clinical utility. Employing a human-centered design approach can enhance the design process and address user-specific needs.
Objective
To establish a proof-of-concept of the human-centered design approach by refining the NewGait® exosuit device for post-stroke gait rehabilitation.
Methods
Using iterative design sprints, the research focused on understanding the perspectives of clinicians, stroke survivors, and caregivers. Two design sprints were conducted, including empathy interviews at the beginning of the design sprint to integrate end-users’ insights. After each design sprint, the NewGait device underwent refinements based on emerging issues and recommendations. The final prototype underwent mechanical testing for durability, biomechanical simulation testing for clinical feasibility, and a system usability evaluation, where the new stroke-specific NewGait device was compared with the original NewGait device and a commercial product, Theratogs®.
Results
Affinity mapping from the design sprints identified crucial categories for stakeholder adoption, including fit for females, ease of donning and doffing, and usability during barefoot walking. To address these issues, a system redesign was implemented within weeks, incorporating features like a loop-backed neoprene, a novel closure mechanism for the shoulder harness, and a hook-and-loop design for the waist belt. Additional improvements included reconstructing anchors with rigid hook materials and replacing latex elastic bands with non-latex silicone-based bands for enhanced durability. Further, changes to the dorsiflexion anchor were made to allow for barefoot walking. Mechanical testing revealed a remarkable 10-fold increase in durability, enduring 500,000 cycles without notable degradation. Biomechanical simulation established the modularity of the NewGait device and indicated that it could be configured to assist or resist different muscles during walking. Usability testing indicated superior performance of the stroke-specific NewGait device, scoring 84.3 on the system usability scale compared to 62.7 for the original NewGait device and 46.9 for Theratogs.
Conclusion
This study successfully establishes the proof-of-concept for a human-centered design approach using design sprints to rapidly develop a stroke-specific gait rehabilitation system. Future research should focus on evaluating the clinical efficacy and effectiveness of the NewGait device for post-stroke rehabilitation.
Background
Stroke is the leading cause of long-term adult disability worldwide [1]. By 2030, nearly 4% of the US population is expected to have had a stroke, leading to an estimated cost burden of ∼$184 billion [2]. While some level of spontaneous biological recovery can occur after a stroke, this process is often incomplete, leaving most stroke survivors with persistent gait impairments, which can lead to walking disabilities, falls, and reduced health-related quality of life [3, 4]. As a result, clinicians emphasize the restoration of gait and balance as a central goal of stroke rehabilitation.
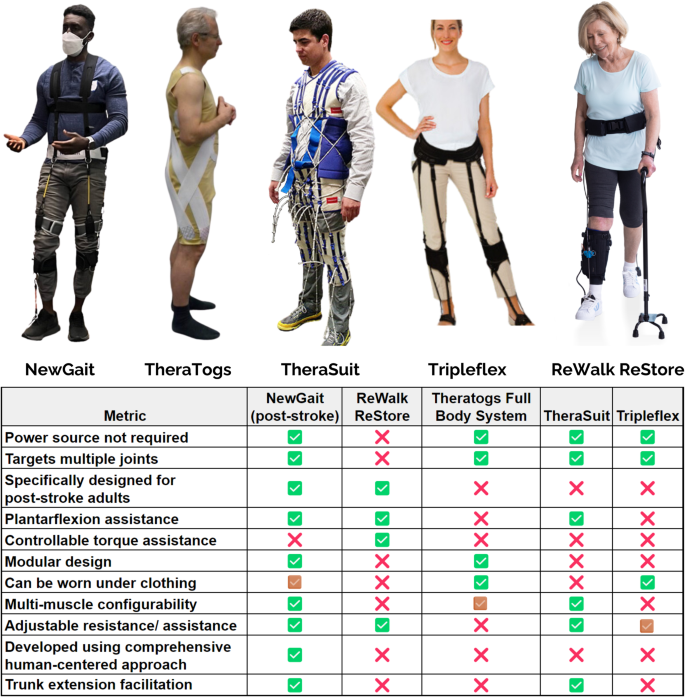
Numerous innovative therapeutic approaches, such as body weight supported treadmill training and robotic therapy, have emerged to address this challenge [5, 6]. However, the outcomes of these interventions have frequently fallen short of expectations, in part due to their high costs and modest benefits, limiting their clinical translation [7, 8]. Recognizing the pressing need for effective, efficient, and low-cost technologies for gait rehabilitation after stroke, researchers and engineers have explored various wearable solutions. Conventional ankle-foot orthoses (AFOs) offer simplicity and affordability, but they may inadvertently result in disuse atrophy and reduced gait efficiency by limiting Achilles tendon excursion and propulsive forces during walking [9, 10]. Moreover, they primarily target the ankle joint, overlooking the essential roles of the hip, knee, and trunk in gait and balance [11]. While devices like TheraTogs [12] and TheraSuit [13] aim to address multiple joint areas, their primary focus on the pediatric market [14] raises challenges when adapting to the adult stroke population (see Fig. 1). TripleFlex [15], a more recent development, targets foot drop and leg-lift deficiencies by putting energy into flexing each joint during the swing phase of gait, thereby offering potential improvements, particularly for adults with neurological conditions like stroke. Additionally, the ReWalk ReStore, while developed specifically for post-stroke gait rehab, only targets the muscles in the shank and requires the user to carry a battery pack on their back [16, 17]. More importantly, most of the existing devices do not offer modularity (i.e., the ability to select and choose different joints) and configurability (i.e., the ability to target different muscle groups) based on patient-specific deficits. Nonetheless, the scarcity of comprehensive studies assessing these devices’ efficacy and effectiveness leaves substantial uncertainties regarding the clinical utility and usability of these devices for stroke rehabilitation.
A recurring issue in the field is that many of these devices have been conceived without adequate input from the individuals who matter most in the rehabilitation process—stroke survivors, their caregivers, and the clinicians providing care. This omission has led to devices that often do not fully align with the actual needs and preferences of these end-users [18,19,20]. As a result, the utilization of these devices remains limited, and questions linger about how well they address the needs and desires of clinicians and patients, further hindering their clinical utility and usability.
Addressing these challenges necessitates a shift in the approach to device development strategies. Integrating the principles of human-centered design can significantly enhance the development process and result in more inclusive, tailored, and empowering solutions [21, 22]. Human-centered design emphasizes understanding people’s needs, motivations, and concerns while engaging stakeholders from the outset and adopting a systems approach to generalize individual interests to collective solutions [23]. It allows for more effective and efficient design by engaging with users early in the development process, yielding valuable insights while working with prototypes and sketches, rather than fully built products, which can prevent the misallocation of resources [24].
In this study, we employ a novel device design framework based on human-centered design strategies, known as “design sprints” [25], to comprehensively grasp user needs and expectations in order to refine a low-cost, passive exosuit device called NewGait device for stroke rehabilitation [26,27,28]. The NewGait device (see Fig. 1), originally developed as a sports and performance enhancement device called SpeedMaker®, features lightweight elastic bands, leg straps, a shoulder harness, a waist belt, and movable anchor points for connecting the bands, rendering it highly modular. These elastic bands not only work in concert with muscle and tendon groups to assist or resist motion, but also aid in providing neuromuscular cues essential to neuroplasticity. Additionally, the elastic nature of the bands helps to facilitate proprioceptive feedback for users [29].
While the clinical efficacy of the NewGait device has not been extensively documented, many clinicians have used it to treat gait and balance issues in individuals with stroke and have anecdotally reported noteworthy clinical improvements. However, feedback from clinicians and patients revealed the need for refinement, particularly for stroke-specific populations, as the original device was not intended for this population. Therefore, the purpose of this study was to use human-centered design approaches to tailor the NewGait device to the unique requirements of stroke rehabilitation. We hope that by prioritizing the input and feedback of stroke survivors, caregivers, and clinicians, we will be able to ultimately enhance its clinical usability and effectiveness in improving the lives of those affected by this debilitating condition.
No comments:
Post a Comment