Sonification has been written about for 8 years. It is about time for our fucking failures of stroke associations to step up to the plate and write a stroke protocol on this. I can guarantee this won't occur.
Hand rehabilitation with sonification techniques in the subacute stage of stroke
Abstract
After a stroke event, most survivors suffer from arm paresis, poor motor control and other disabilities that make activities of daily living difficult, severely affecting quality of life and personal independence. This randomized controlled trial aimed at evaluating the efficacy of a music-based sonification approach on upper limbs motor functions, quality of life and pain perceived during rehabilitation. The study involved 65 subacute stroke individuals during inpatient rehabilitation allocated into 2 groups which underwent usual care dayweek) respectively of standard upper extremity motor rehabilitation or upper extremity treatment with sonification techniques. The Fugl-Meyer Upper Extremity Scale, Box and Block Test and the Modified Ashworth Scale were used to perform motor assessment and the McGill Quality of Life-it and the Numerical Pain Rating Scale to assess quality of life and pain. The assessment was performed at baseline, after 2 weeks, at the end of treatment and at follow-up (1 month after the end of treatment). Total scores of the Fugl-Meyer Upper Extremity Scale (primary outcome measure) and hand and wrist sub scores, manual dexterity scores of the affected and unaffected limb in the Box and Block Test, pain scores of the Numerical Pain Rating Scale (secondary outcomes measures) significantly improved in the sonification group compared to the standard of care group (time*group interaction < 0.05). Our findings suggest that music-based sonification sessions can be considered an effective standardized intervention for the upper limb in subacute stroke rehabilitation.
Introduction
After a stroke event, most survivors (80–90%) suffer from arm paresis, poor motor control and other disabilities, which evolve in a chronic condition in about 30–40% of cases2. Consequently, patients have difficulty in performing activities of daily living, a fact that severely affects their quality of life and independence3. Task-oriented sensory-motor training, which allows to transmit the sensory information of the feedback to the central nervous system during task execution, and movements adaptation, is recognized as significant in increasing post-stroke arm function and dexterity2,4. Beside other factors, such as patient’s compliance and subjective interest in stimulus, the intensity of training and patient’s motivation have been indicated as key features for a successful rehabilitation therapy5,6.
The development of technologies for rehabilitation has made it possible to formulate new application paradigms obtained by integrating the current rehabilitation pathways with instrumental interventions7,8. Sensory-motor rehabilitation techniques, obtained through technological devices (such as virtual reality, robots, non-invasive stimulations , motion capture) and used in support of traditional rehabilitation techniques, seem to provide objective parameters for patient evaluation, accelerate the process of motor recovery and improve motor performance at discharge by means of a top-down approach9,10.
Although the results obtained with the currently available devices are encouraging, we are only at an early stage for the exploitation of these technologies. In fact, while technology-assisted rehabilitation of the upper limb has demonstrated to have a significant impact on motor outcomes, especially at the proximal level (shoulder and elbow)11, the functional recovery of the hand (in particular of the prehension function) still presents some issues12,13.
Music and its elements (especially the rhythm) are widely used in rehabilitation14.This is due to the activation of the neuronal networks, in the limbic and paralimbic areas, and in the brain areas involved in movement (motor cortex, supplementary motor area, cerebellum, basal ganglia, etc.)15,16. Many studies document the possibility that exposure to music during training, but, also through specific rehabilitation interventions, may induce plastic changes15,16,17,18,19 in the sensory-auditory circuits and motor areas20,21. These changes, resulting in a neuronal reorganization in the nodal points of the brain networks and in fiber bundles, can determine effects lasting beyond the actual duration of the rehabilitation intervention15. Moreover, music in the rehabilitation process determines an emotional involvement, creating a strong motivational basis15,16.
The recent literature shows how the use of music in stroke rehabilitation can improve gait (speed, cadence and step length, balance)22,23, movement of the upper limbs24,25, language26,27, but also mood and other psychological aspects28,29,30. More recent studies use, for the rehabilitation of the upper limbs, the mapping of the patient’s movements to whom a sonorous stimulus is associated (sonification)31,32,33,34. Sonification can improve motor functions rehabilitation and can facilitate the integration of auditory and sensory-motor systems35,36,37. This technique can also strengthen and support the damaged proprioceptive system and can make the rehabilitative process more pleasant and stimulating from an emotional and motivational point of view15,37. In some studies, the kinematic data of the gesture are translated into modulations of some parameters (typically frequency and amplitude) of a continuous synthetic sound38,39,40.
In other post-stroke hand rehabilitation studies, the sonification action was based on the execution of short scales or melodic intervals that the patient had to reproduce through specific movements, with the final goal of creating "simple nursery rhymes or other familiar tunes", modulating music timbre and intensity41. Further, Reh et al.42 supported the rehabilitation of walking by a combination of an ecological sound (noise produced by a step in the snow) together with a predetermined glissando effect.
In this study the sonification can be considered as a properly selected set of sonorous-music stimuli activated by patient’s movements with the mediation of a sensor (in this specific case the Leap Motion Controller). Synthesized sounds/musical texture and their parameters (mainly rhythm, pitch/melody, intensity/dynamics, harmony and timbre) are used to represent movements characteristics, especially from a temporal and spatial point of view. Sonification makes possible the improvement of sensorimotor learning, proprioception, movements planning and execution37.
In particular music elements used in this study were automatically associated to the patient’s movements without involvement of any cognitive tasks. This allows the patient to focus attention mainly on the motor outcome. In particular, given the importance of hand functions in activities of daily living and manipulation, the protocol (Sonichand) was developed and validated for the training of pronation and supination of the forearm, ulnar and radial deviation of the wrist and hand grasping movements43.
The main objective of this randomized controlled study conducted in subacute stroke patients during inpatient rehabilitation, was to verify the effectiveness (evaluated through the assessment of the upper limb level of impairment at baseline and end of treatment) of a new rehabilitative hand treatment based on a musical sonification approach compared to a conventional intervention. The secondary aim was to evaluate if this technique could be beneficial for reduction of pain perceived during training and improve the patient's perceived quality of life. The main hypothesis of this study was that our sonification approach could be more effective than a conventional intervention for the rehabilitation of subacute stroke patients, especially for the recovery of hand motor function.
Results
Clinical characteristics of the sample at baseline are reported in Table 1. Two patients allocated to the Sonification Group interrupted the trial between T0 and T2: the first one worsened his/her clinical condition and the second one was hospitalized. In addition, 18 patients in the Sonification Group and 16 patients in the Standard of Care Group were lost to follow-up due to the clinical worsening (2 patients in the Sonification Group and 3 patients in the Standard of Care Group) or to the difficulty to go back to the rehabilitative centers after the end of the interventions (16 patients in the Sonification Group and 13 patients in the Standard of Care Group) (Flow Diagram is reported in Fig. 1). No side effects were observed in both the experimental and control groups after training.
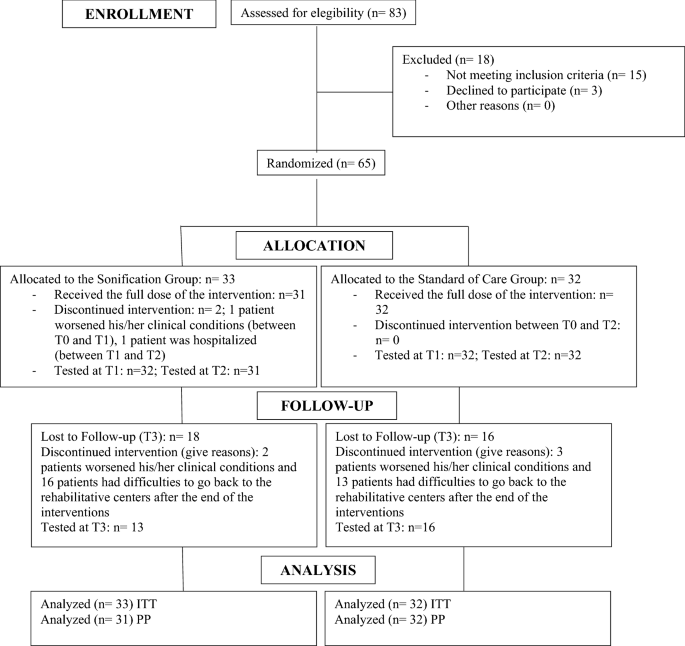 |
The flow chart of the study. All randomized patients received the allocated intervention. Between baseline and the 4-week evaluation two patients in the Sonification group discontinued the treatment. No discontinuation occurred in the Standard Care Group. After 1 month from the beginning of treatment (T3 follow-up) 18 and 16 patients were lost to follow-up in the Sonification and Standard Care Groups, respectively. The primary analysis (T2, end of the 4-week treatment) was performed on the Intention To Treat (ITT) and Per Protocol (PP) populations, with the numbers reported in the figure.
Primary outcome
The upper limb impairment assessed by the Fugl-Meyer Upper Extremity scale total score44 , showed a significantly greater improvement between T0 and T2 (Table 2, Fig. 2) in the Sonification Group compared to the Standard of Care Group (time*group interaction: p = 0.024), as pointed out by the Intention To Treat analysis.
No comments:
Post a Comment