Notice that the stroke medical world knows ABSOLUTELY NOTHING about gait rehab. They can get you moving but not recovered. So a complete failure by your stroke medical professionals. I don't consider using compensatory efforts to walk a success.
These legs were made for propulsion: advancing the diagnosis and treatment of post-stroke propulsion deficits
Journal of NeuroEngineering and Rehabilitation volume 17, Article number: 139 (2020)
Abstract
Advances in medical diagnosis and treatment have facilitated the emergence of precision medicine. In contrast, locomotor rehabilitation for individuals with acquired neuromotor injuries remains limited by the dearth of (i) diagnostic approaches that can identify the specific neuromuscular, biomechanical, and clinical deficits underlying impaired locomotion and (ii) evidence-based, targeted treatments. In particular, impaired propulsion by the paretic limb is a major contributor to walking-related disability after stroke; however, few interventions have been able to target deficits in propulsion effectively and in a manner that reduces walking disability. Indeed, the weakness and impaired control that is characteristic of post-stroke hemiparesis leads to heterogeneous deficits that impair paretic propulsion and contribute to a slow, metabolically-expensive, and unstable gait. Current rehabilitation paradigms emphasize the rapid attainment of walking independence, not the restoration of normal propulsion function. Although walking independence is an important goal for stroke survivors, independence achieved via compensatory strategies may prevent the recovery of propulsion needed for the fast, economical, and stable gait that is characteristic of healthy bipedal locomotion. We posit that post-stroke rehabilitation should aim to promote independent walking, in part, through the acquisition of enhanced propulsion. In this expert review, we present the biomechanical and functional consequences of post-stroke propulsion deficits, review advances in our understanding of the nature of post-stroke propulsion impairment, and discuss emerging diagnostic and treatment approaches that have the potential to facilitate new rehabilitation paradigms targeting propulsion restoration.
Introduction
THE fast, economical, and stable gait that is characteristic of healthy bipedal locomotion [1–6] requires the coordination of three locomotor subtasks—propulsion, limb advancement, and bodyweight support. During the propulsion locomotor subtask, positive work by the trailing limb accelerates the body into the next gait cycle [7]. To walk faster, people with intact neural control symmetrically increase the positive work performed by each limb [8–10]. The coordinated modulation of the work performed by each limb leverages the natural oscillatory dynamics that arise from repeating foot-ground interactions to optimize stability and economy of effort while regulating walking speed [6, 10]. In contrast, the hemiparetic gait observed after stroke [11–13] is slow [14–17], metabolically expensive [10, 15, 18–20], and unstable [21–24]. In neurologically unimpaired individuals, the plantarflexor muscles are the primary generators of positive work [9]; however, post-stroke neuromotor deficits result in a distal-to-proximal redistribution of the positive work generated by the muscles of the paretic limb [10, 25, 26], and, ultimately, a markedly altered profile for the anterior ground reaction force (i.e., the propulsion force) [27].
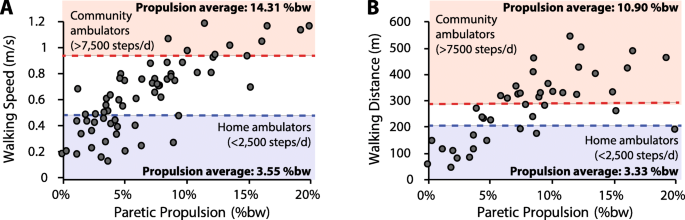
Conventional post-stroke rehabilitation efforts have had limited effectiveness in restoring the propulsion function inherent to a healthy bipedal gait, with functional improvements often being the product of compensatory mechanisms [26, 28, 30, 31]. The propulsion deficits that persist across the months and years post-stroke constrain long-term outcomes and contribute to a sedentary lifestyle, physical inactivity, and poor health [15, 32–37]. Indeed, post-stroke propulsion deficits are associated with a slow walking speed [17] and reduced long distance walking ability [38]—key predictors of real-world ambulatory activity in the home and community [33, 39, 40]. Examination of data reported in previous studies [17, 28, 29] demonstrates that functional speeds and distances are rare in those with little propulsion output from their paretic limbs. Indeed, people post-stroke who walk at the speeds and distances indicative of unlimited community ambulation (i.e., more than 7500 steps/d) [39] have relatively high levels of paretic propulsion (Fig. 1). More specifically, those who walk faster than 0.93 m/s—a walking speed that identifies individuals who walk more than 7500 steps/d with a specificity of 80% [39]—walk with an average peak paretic propulsion of 14.31 ±3.70%bodyweight (%bw) (Fig. 1a). Similarly, individuals able to walk farther than 288 m during the 6-minute walk test—a distance with similar discriminative abilities as a short-distance walking speed of 0.93 m/s [39]—walked with an average peak paretic propulsion of 10.90 ±3.62%bw (Fig. 1b). In contrast, those classified as home ambulators (i.e., individuals who walk less than 2500 steps/d) presented with substantially lower paretic propulsion of 3.55 ±2.38%bw and 3.33 ±2.51%bw, respectively.
In this expert review, we discuss recent advances in our understanding of post-stroke propulsion deficits, review emerging approaches to systematically diagnose and treat the underlying impairments, and highlight the substantial research and development effort that is required before these approaches can alter clinical practice. More specifically, the next section on “Propulsion diagnostics” overviews (i) the critical need for point-of-care propulsion diagnostics, (ii) the neurophysiological basis for propulsion impairments, (iii) the heterogeneous impairments underlying post-stroke propulsion deficits, and (iv) the potential for propulsion phenotyping to direct individualized therapies. The following section on “Propulsion treatments” overviews (i) the inadequacy of conventional intervention approaches and (ii) emerging propulsion-focused technologies and interventions that leverage internal and external mechanisms to target the different aspects of propulsion impairment.
No comments:
Post a Comment