Notice the word; 'care' NOT RESULTS OR RECOVERY. In my world only results would be used in determining any honors. Nothing here suggests he was working towards 100% recovery; the only goal in stroke.
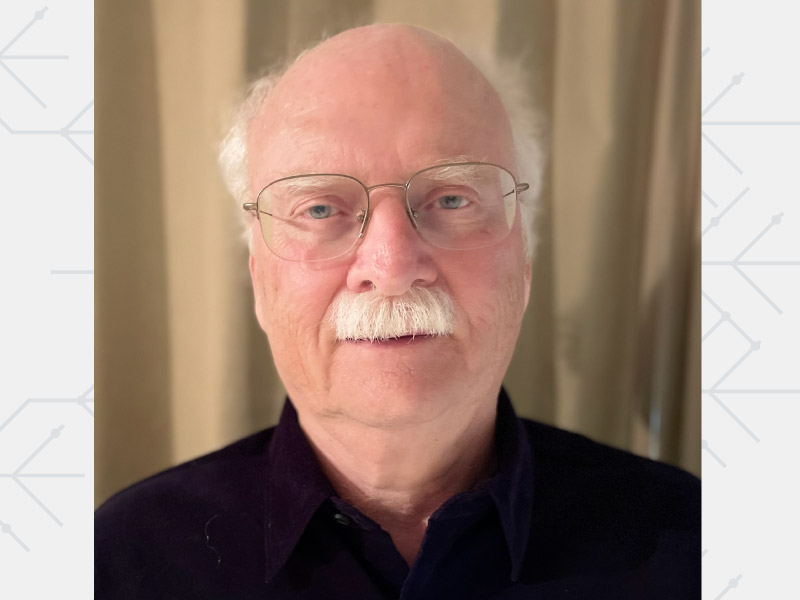
Honoree helped transform acute stroke care - Dr. Marc Fisher
Each year, nearly 800,000 people in the United States experience a stroke — when blood flow to the brain is interrupted. And when it happens, time is of the essence. The impact is swift, with brain cells beginning to die within minutes.
That's why getting a patient evaluated, triaged and treated quickly can mean the difference between a full recovery and significant loss of speech or body function, or death. A major part of the triage is figuring out how much of the brain tissue that lies near the site of the stroke, an area called the ischemic penumbra, can be saved.
Dr. Marc Fisher, a Harvard Medical School professor and a former editor of Stroke, a journal of the American Heart Association, has devoted his career to this aspect of post-stroke care. For this and many other contributions to the field, Fisher will receive the Gold Heart Award, the AHA's highest volunteer honor, at a virtual awards ceremony June 22.
"What we're trying to do is salvage as much of the tissue as possible so that the size of the ultimate damage is as small as possible," Fisher said. "The smaller the damage, the better the outcome is going to be."
Fisher earned his medical degree from the State University of New York at Syracuse and taught at the University of Massachusetts Medical School in Worcester for 36 years as well as serving as the vice chairman of the Department of Neurology. It was there that Fisher and his team realized that they could use diffusion MRI, a magnetic imaging technique, to evaluate stroke patients. Being able to locate viable tissue and large vessel occlusions — strokes that result from a blockage in one of the brain's major arteries — meant that doctors could finally identify patients who could benefit from a relatively simple procedure, known as a thrombectomy, to remove a blood clot in the brain.
"Thrombectomies are dramatically effective," Fisher said. "You can take someone who can't speak or move their right side and they have the clot taken out and within a short time, they are back to normal or pretty close to normal. It's amazing."
In 2010, Fisher became editor-in-chief of the AHA journal Stroke, where he served until his term ended in 2020. There, Fisher developed a trainee reviewer program both in the U.S. and overseas that taught younger scientists how to critically evaluate and write research papers. He also oversaw the launch of the journal's social media presence that sought to engage with scientists and patients around the world. And under Fisher's leadership, the journal implemented a preclinical checklist to improve the quality of published work.
In addition to teaching at Harvard Medical School, today Fisher is a member of the neurology faculty at Beth Israel Deaconess Medical Center in Boston and serves as president of the World Stroke Organization(I see the WSO as useless for stroke survivors; NO PROTOCOLS for recovery.), whose mission is to educate health care professionals and the public to improve stroke care around the world.
Fisher has published prolifically, with more than 300 peer-reviewed papers, and served as a mentor to a long line of medical residents and stroke research fellows, many of whom today hold prestigious positions around the world. He has also collaborated with some of the top researchers in the field of MRI, such as the late Christopher Sotak of Worcester Polytechnic Institute, and Steve Warach of the University of Texas at Austin, relationships that he said were crucial to his success.
The field of acute stroke care has made tremendous strides over the past 25 years,(I don't see this at all, only 10% get to full recovery, only 12% get to full recovery using tPA. THAT IS COMPLETE FAILURE IN ANY BUSINESS!) but a lot of work remains. One new area of research is alternative treatments for people who don't qualify for a thrombectomy because the blockage is hard to reach or because they don't live close to a hospital where the procedure is performed.
Despite progress, stroke remains a leading cause of death in the U.S., according to the Centers for Disease Control and Prevention. That's why Fisher urges everyone to learn the signs, including drooping face, limp arm and slurred speech, and reminds them that every minute counts. One easy way to remember is by using the F.A.S.T. acronym, which stands for face, arm, speech and time.
"You need to recognize if you or a family member is having a stroke and seek care in an emergency room right away because the faster you get care, the better chance we have to help you," Fisher said.
No comments:
Post a Comment