You mention limited guidance on the use of these but don't actually solve the problem.
1. What is the objective diagnosis that would indicate use of each one of these.
2. What is the EXACT PROTOCOL for their use?
3. What is the expected result from following that protocol?
A framework for clinical utilization of robotic exoskeletons in rehabilitation
Journal of NeuroEngineering and Rehabilitation volume 19, Article number: 115 (2022)
Abstract
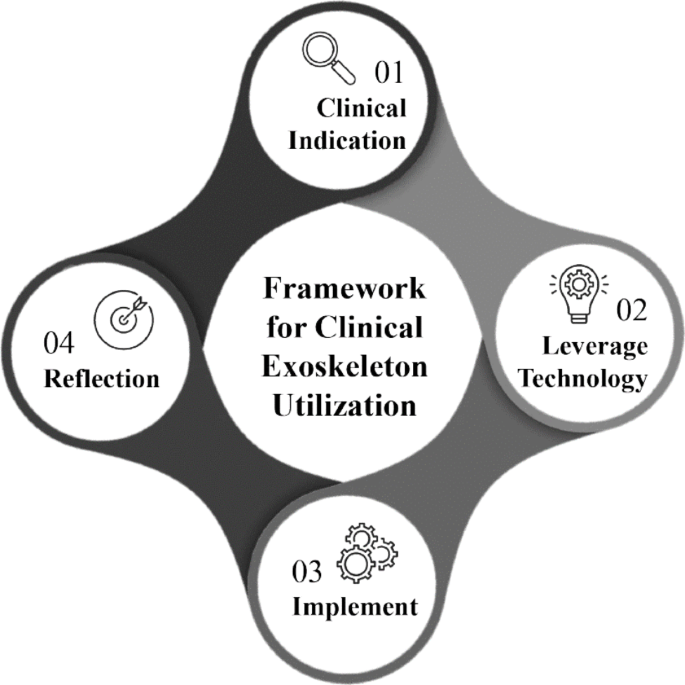
Exoskeletons are externally worn motorized devices that assist with sit-to-stand and walking in individuals with motor and functional impairments. The Food & Drug Administration (FDA) has approved several of these technologies for clinical use however, there is limited evidence to guide optimal utilization in every day clinical practice. With the diversity of technologies & equipment available, it presents a challenge for clinicians to decide which device to use, when to initiate, how to implement these technologies with different patient presentations, and when to wean off the devices. Thus, we present a clinical utilization framework specific to exoskeletons with four aims.
These aims are to assist with clinical decision making of when exoskeleton use is clinically indicated, identification of which device is most appropriate based on patient deficits and device characteristics, providing guidance on dosage parameters within a plan of care and guidance for reflection following utilization. This framework streamlines how clinicians can approach implementation through the synthesis of published evidence with appropriate clinical assessment & device selection to reflection for success and understanding of these innovative & complex technologies.
Background
The evolution towards evidenced based practice in physical therapy has progressed over the past 25 years, however many barriers to effective translation to clinical practice persist [1]. One critical barrier is when a novel intervention or technology is introduced, there is a paucity of evidence and processes to guide clinicians on how it can be integrated into their everyday clinical practice.
In the current manuscript, we will discuss the clinical use of robotic exoskeletons, which have come into commercial availability since 2011. In the context of this manuscript, exoskeletons are defined as externally worn devices that assist with sit-to-stand and gait training in individuals with motor and functional impairments. They have tremendous potential to assist in the delivery of rehabilitative care through improved efficiency, decreased cost with ability to achieve a high stepping dosage and intensity, and decreased therapist-burden and risk of injury compared to other gait training strategies [2, 3]. The field of robotic technologies is rapidly evolving, with a projected growth of 26% over the next 5 years [4]. Exoskeletons currently approved for clinical use by the US FDA include RewalkTM, Ekso™, Indego™, Hybrid Assistive Limb (HAL) TM for medical use (lower limb type), Rewalk Restore™, B-Temia Keeogo + ™ and Honda Walking Assist Device (WAD)TM.(5, 6) Table 1 describes the FDA-approved device features including level of assistance, resistance modulation, joint control, type of feedback, and stepping actuation. Exoskeletons currently are not considered standard of care in rehabilitation, however patients often seek facilities offering these advanced technologies. Given the emerging evidence of clinical utility, patient interest, and anticipated growth of the field, it is critically important clinicians can effectively evaluate and implement the use of these devices.
B LE = bilateral lower extremity device, U LE = unilateral lower extremity device, FP = fully powered; device provides majority of power at joints and user needs little to no volitional strength to utilize; PA = partially assistive; device provides customized partial assistance to augment deficits to improve gait.
Depending on the rehabilitation facility, clinicians may have access to only one of these devices while others may have multiple options. Regardless of the device availability, practitioners must systematically assess the technology’s features related to their patient’s impairments and functional level to determine if utilization is indicated. Table2 describes the outcomes from randomized control trials to date that have focused on use of FDA approved devices compared to conventional care.
Specifically, this manuscript focuses on diagnoses approved for use by the FDA. Studies which have investigated the sub-acute and chronic stroke populations included persons with single or unilateral stroke, with a majority including individuals greater than 55 years of age [7,8,9,10,11, 14, 15]. In the incomplete spinal cord injury (SCI) population, most investigations are single group interventional studies or pilot randomized trials. These studies mostly focus on inclusion of participants with incomplete (AIS C or D) injuries with upper motor neuron signs and sufficient upper extremity strength to use an assistive device. Studies focusing on participants with cervical level injuries, AIS A and B injury classification, and lower motor neuron injuries are limited and with varying sample sizes of 9–52 subjects [12, 13]. It should be noted, the aim in many of these studies was to obtain FDA approval with a primary focus on establishing safety with one primary efficacy outcome. Thus in many cases, the true functionality and clinical effectiveness of these devices has not been investigated. Furthermore, these studies also do not focus on dosing, progression strategies, or rehabilitation principles critical to therapeutic intervention [16,17,18].
Adding more uncertainty to application of the available literature, the clinical practice guideline (CPG) for improving walking function in chronic neurological diagnoses, recommended against utilizing robotic interventions [17]. Ten of the eleven studies referenced were not the FDA approved devices focused on in this current manuscript, and eight of the studies focused on treadmill-based robots, specifically the Lokomat [17] These conclusions should be taken with caution, given the substantial differences in functionality and physical demand between the treadmill-based robots and the overground exoskeletons of current focus. Thus, understanding the current literature along with synthesis of knowledge from clinical experience regularly utilizing exoskeletons in practice was critical in developing this framework.
In this four-step framework, we focus specifically on clinical application, rather than exoskeleton use for personal mobility. As authors, we are in a unique position to propose a comprehensive framework to assist in this systematic evaluation due to having extensive experience utilizing a wide array of these exoskeletons during the research and development phase, FDA clinical trials, as well as extensive use in everyday clinical practice [2, 11, 14, 19, 20].
Step 1: Clinical indications for exoskeleton use
Clinicians performing evaluations may identify a patient is suitable for exoskeleton utilization at the beginning of an episode of care, or when challenges arise during gait training within a conventional plan of care. Often a patient’s clinical presentation does not match the exact inclusion/exclusion criteria described in the published literature. This should not preclude a clinician from considering incorporation of exoskeleton technology in the plan of care. Inclusion criteria can serve as a baseline for understanding which patient populations and presentations have been investigated to date. Because technology and software development often outpace scientific research, frequently the device investigated is an older version with fewer features or modes than what is available currently.
No comments:
Post a Comment