I think you're in denial about survivor involvement in stroke 'care(NOT RECOVERY!)
If it existed, I'm sure one of my many readers would have commented on it.
Survivors are still considered laboratory rats.
For the past five years Amy Farber has been battling not only her own disease but also the wall of resistance erected by those who believe that a patient can make about as much of a meaningful contribution to the process of scientific discovery as a laboratory rat.
Patient Partnership in Stroke Care: A Scoping Review
Introduction & Background
Patient partnership in healthcare is increasingly recognized as essential for improving patient outcomes and experiences. The King’s Fund defines patient partnership as a collaborative relationship where power is shared between clinicians and patients, moving beyond traditional hierarchical dynamics [1]. Patient experience, a key component of quality healthcare, is defined as ‘what the process of receiving care feels like for the patient, their family and carers’ [2]. Across global healthcare systems, the most effective healthcare experiences are shaped through strong patient-clinician relationships that emphasize respect, autonomy, continuity, and education [3].Historically, healthcare models positioned clinicians as the sole decision-makers, reinforcing the misconception that only medical professionals hold the knowledge to guide treatment. However, since the 2014 NHS Five-Year Forward View, patient partnership has become the central focus of the NHS [4]. This shift represents a significant transformation in the role of patients in decision-making and care delivery. While many theoretical models of patient partnership have been developed, research on the practical application, particularly in improving patient experience, remains limited. This review will unpack the definition of patient partnership within the context of stroke care and explore how medical education, particularly at the undergraduate level, can transition from a transactional process to one that promotes partnership and shared decision-making with patients.
Why focus on stroke care?
Stroke is one of the leading causes of death and disability in the UK, with over 113,000 strokes occurring annually [5,6]. Although approximately 80% of stroke patients survive their hospital stay, many continue to experience long-term challenges [7,8]. With over 1.3 million stroke survivors in the UK, this number is expected to rise as the population ages and treatment methods develop [7,9]. Despite extensive research into the pharmacological and surgical management of stroke, the role of patient partnership in stroke recovery and long-term care remains underexplored.
Many stroke survivors report unmet long-term needs, particularly in activities of daily living (ADLs), home adaptations, and financial support [10]. A recent study found that nearly half of the stroke survivors in the UK had at least one unmet need following their stroke [10]. Addressing these gaps requires a patient partnership approach, ensuring survivors are actively engaged in their recovery and rehabilitation.
The Stroke Association recognises patient involvement as critical in improving stroke outcomes [11]. One of the top five research priorities in stroke care is delivering evidence-based treatment to improve survival and quality of life [10,12]. Studies suggest that patient engagement improves treatment adherence, functional outcomes, and overall satisfaction with care [13]. Given the increasing number of stroke survivors, integrating patient partnership within stroke care is not only beneficial but necessary to optimise recovery and long-term well-being.
The patient partnership model
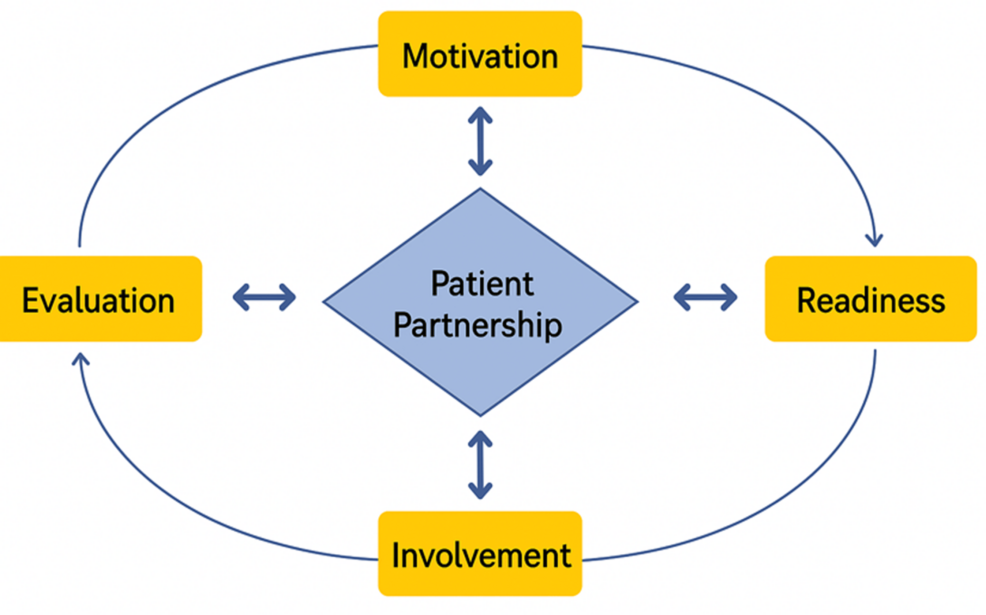
The patient partnership model has four stages: motivation, readiness, involvement, and evaluation [14], as summarised in Figure 1. Motivation involves the clinician and patient recognising the condition and the importance of active engagement [14]. Readiness focuses on preparing the patient with knowledge, allowing for active participation [14]. Involvement ensures continued collaboration to enhance health outcomes and quality of life [14]. Finally, regular evaluation assesses and strengthens the partnership for sustained and optimal outcomes [14].
Patient partnership: A life-long journey
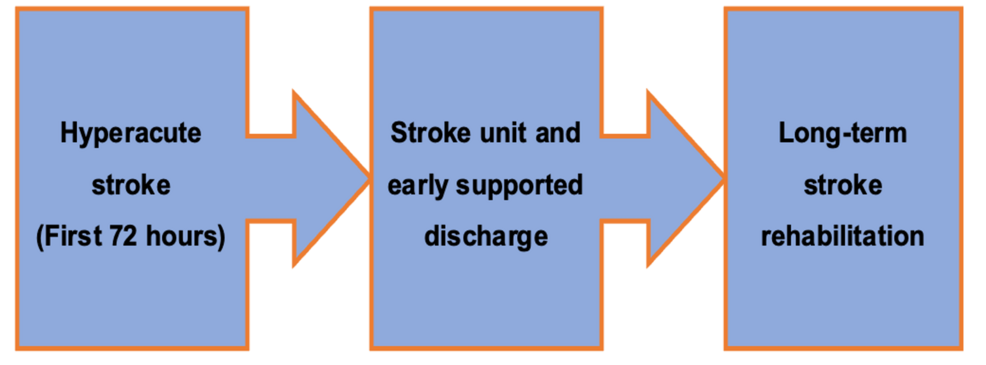
Collaboration between healthcare professionals and patients with stroke is a lifelong process. Understanding key interactions throughout the patient’s journey is essential for developing long-term engagement. This review will explore the role of patient partnership at each stage of the Stroke RightCare Pathway as summarised in Figure 2 [15]. This pathway is a national framework designed to improve stroke care in the UK through collaborative approaches [15]. By using the Stroke RightCare Pathway as the foundation of this review, we aim to demonstrate a holistic approach to integrating patient partnership and its impact on the stroke patient’s journey.
Review
Methodology
A comprehensive scoping review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16], as illustrated in Figure 3. The search was conducted using three databases: the Cochrane Library, Embase, and PubMed. The search strategy was designed to identify studies that explored patient partnership in stroke care, as well as the role of medical education in embedding these principles into clinical practice. The search terms are summarised in Table 1.
No comments:
Post a Comment