How soon will your doctor inform you of this treatment?
MRI reveals how statins reduce vessel wall inflammation
Statin use decreases vertebrobasilar dissecting aneurysms (VBDA) wall enhancement identified on vessel wall (VW) MRI scans, researchers have found.
The findings offer further evidence that statins reduce stroke risk, wrote a team led by Yisen Zhang, MD, of Beijing Tiantan Hospital and Beijing Neurosurgical Institute at Capital Medical University in China.
"Among patients with unruptured vertebrobasilar dissecting aneurysms, statins reduced aneurysm wall enhancement, reduced the levels of circulating inflammatory biomarkers, and stabilized intramural hematomas," the group noted.
VBDAs are significant causes of stroke, and aneurysm wall enhancement at the vessel wall, as identified on MRI, is a marker of inflammation that suggests vulnerability to VBDAs. Although previous research has shown that statins may reduce inflammation in intracranial saccular aneurysms, their effect on VBDAs has been unclear.
Zhang and colleagues conducted a study that evaluated the effect of a six-month atorvastatin treatment on VBDA wall enhancement as seen on vessel wall MRI scans. The research included 40 participants with unruptured VBDAs between July 2021 and January 2023. Patients were randomized one-to-one into a daily 20 mg atorvastatin group and a control group; all underwent VW MRI at the study start and at six-month follow-up. The primary outcome was any change in aneurysm wall enhancement measured by the quantitative wall enhancement index, or WEI (which evaluates rupture risk of intracranial aneurysms), and three-dimensional wall enhancement volume rate, or WEVR (which evaluates the growth and instability of intracranial or aortic aneurysms). Secondary outcomes were changes in aneurysm size or structure and any inflammation-related biomarkers.In the statin group, both the WEI and WEVR of the aneurysm wall decreased at six months MR imaging compared with those measures at baseline. Between baseline and follow-up, the change in WEI was -0.3 in the statin group and 0.1 in the control group (p < 0.001), while the change in WEVR was -15.1% in the statin group and 5.3% in the control group (p < 0.001). Circulating plasma levels of C-reactive protein, tumor necrosis factor alpha, interleukin-6, and interleukin-1 beta all decreased in the atorvastatin group compared with the control group (all p < 0.05). The atorvastatin group also showed slowed progression of intramural hematoma (304 mm3 compared with 100.3 mm3 in the control group; p = 0.006). 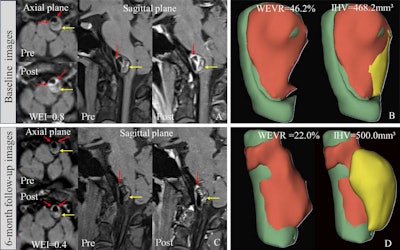 Typical statin case presentation. Images were obtained in a 35-year-old woman with a left vertebral artery dissection aneurysm who presented with headache. (A, C) Vessel wall MRI scans show aneurysm wall enhancement. (B, D) Panels show three-dimensional postprocessed images derived from contrast-enhanced T1-weighted MRI scans, illustrating the wall enhancement volume ratio (WEVR) and intramural hematoma volume (IHV) calculated using 3D Slicer (version 5.0.3; Slicer Community, www.slicer.org). (A) Precontrast and postcontrast images in the axial and sagittal planes at baseline MRI show aneurysm wall enhancement, with a wall enhancement index (WEI) of 0.8. (B) Image shows the WEVR and intramural IHV at baseline (WEVR = 46.2%; IHV = 468.2 mm3). (C) Precontrast and postcontrast images in the axial and sagittal planes at the 6-month follow-up show aneurysm wall enhancement, with a WEI of 0.4. (D) Image obtained at the 6-month follow-up (WEVR = 22%; IHV = 500 mm3). The yellow arrows in A and C indicate the intracranial hematoma, and the red arrows indicate wall enhancement. Red areas in B and D show the enhanced wall, green areas highlight the nonenhanced wall, and yellow areas highlight the IHV. RSNA
Typical statin case presentation. Images were obtained in a 35-year-old woman with a left vertebral artery dissection aneurysm who presented with headache. (A, C) Vessel wall MRI scans show aneurysm wall enhancement. (B, D) Panels show three-dimensional postprocessed images derived from contrast-enhanced T1-weighted MRI scans, illustrating the wall enhancement volume ratio (WEVR) and intramural hematoma volume (IHV) calculated using 3D Slicer (version 5.0.3; Slicer Community, www.slicer.org). (A) Precontrast and postcontrast images in the axial and sagittal planes at baseline MRI show aneurysm wall enhancement, with a wall enhancement index (WEI) of 0.8. (B) Image shows the WEVR and intramural IHV at baseline (WEVR = 46.2%; IHV = 468.2 mm3). (C) Precontrast and postcontrast images in the axial and sagittal planes at the 6-month follow-up show aneurysm wall enhancement, with a WEI of 0.4. (D) Image obtained at the 6-month follow-up (WEVR = 22%; IHV = 500 mm3). The yellow arrows in A and C indicate the intracranial hematoma, and the red arrows indicate wall enhancement. Red areas in B and D show the enhanced wall, green areas highlight the nonenhanced wall, and yellow areas highlight the IHV. RSNA
No comments:
Post a Comment