Because your incompetent? doctor and hospital didn't get you 100% recovered, you're going to need massive amounts of resilience to do everything on your own!
Good word salad but NOTHING SUGGESTING WORKING ON 100% RECOVERY!
What the survivor has to do but NOTHING FOR THE THERAPISTS, DOCTORS OR HOSPITAL! This is why survivors need to be in charge; they'll never take their eyes off the only goal in stroke; 100% recovery!
Living with Life After Stroke: Navigating Rehabilitation, Relationships, Resilience
Key words: Stroke Survivorship, Rehabilitation, Caregiver, Resilience.
Introduction
Stroke is one of the most common and significant causes of death and disability globally, and the longterm effects of this condition go far beyond the period of hospitalisation. Stroke is the fourth major cause of death and the fifth major cause of disability in India.1 The Global Burden of Disease (GBD) study highlights that stroke was accountable for over 6.6 million deaths and 143 million disability-adjusted life years (DALYs) in 2019.2 Rising frequency of strokes especially in the lowmiddle income countries (LMICs) such as India is due to modifiable risk factors, such as hypertension, obesity, high blood glucose levels, air pollution, and poor diet (Figure 1).3 In fact, 70% of strokes are experienced in LMICs.4 The gender distribution shows that males have an increased incidence than females, although this difference varies by geography and age group (Figure 2).5,6 The survivors of stroke live with some degree of physical, cognitive, and emotional disabilities that linger long after the original medical crisis has taken place. The idea of life after a stroke involves more than medical rehabilitation. It also involves adaptation, resilience, re-establishing selfidentity and redefining familial and social connections in the presence of new constraints. Past studies have discovered that resilience is a key predictor of recovery outcomes.7 But resilience is not created in a vacuum, but is shaped by rehabilitation access, interpersonal support and systems of the healthcare system.
This paper reviews the emerging literature on stroke survivorship to trace a comprehensive trajectory of life after stroke. The research analyses the effects of rehabilitation, relationships, and resilience on patient outcomes. It pays a critical focus on health care systems, policy outlooks, and forthcoming stroke recovery research prospects.
Figure 1: Risk factors of stroke in young adults, highlighting modifiable contributors.
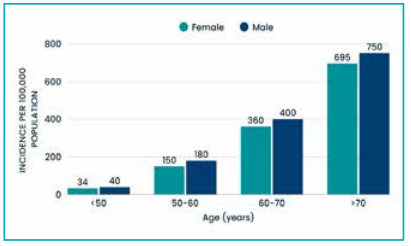
Figure 2: The graph show distinct patterns across different age groups and sexes. Men had a higher incidence of stroke than women in the younger (15–49 years) and middle-aged (50–69 years) groups. However, in the older age group (70+ years), the incidence rates for women approached and were similar to those of men. This indicates that while younger and middle-aged men are more at risk, older women face nearly the same risk of stroke as men.
Source: Behera DK, Rahut DB, Mishra S, et al. Sci Rep. 2024;14(1):22640.6
Rehabilitation Pathways
Rehabilitation serves as the foundation for functional improvement following stroke.
Physical rehabilitation: Physical therapy, occupational therapy and speech-language therapy are the most evidence-based treatments to restore movement, hand skills, and verbal abilities. Early intervention optimises neuroplasticity and increases functional autonomy. Specific regimens frequently incorporate task-specific training, repetitive movement practice, and adaptable equipment. Special emphasis is placed on the investigation of emerging technologies and developments in stroke rehabilitation. From robots, virtual reality and neurostimulation approaches, the evolving landscape of rehabilitation technology presents a great opportunity for improving outcomes and quality of life for stroke patients. These inventions have demonstrated the ability to alter rehabilitation techniques and enhance outcomes for stroke patients.8
Cognitive rehabilitation: The survivor usually has difficulties in their memory, attention and decisionmaking capabilities. The systematic cognitive training techniques enhance thinking skills, concentration, day-to-day activities and quality of life. Research suggests that, in most situations, the challenges with thinking are strongly correlated with loss of independence rather than movement impairment. Cognitive rehabilitation methods, like other rehabilitation concepts, can be divided into two types: restorative and compensatory approaches. Restorative techniques aim to repair or restore degraded function. Compensatory techniques teach and transfer new tactics, skills, or accommodations to compensate for impairments when the original function may not be entirely regained.9
Technological aids: Innovative technological aids are transforming rehabilitation by improving access and engagement. Remote rehabilitation, robotic applications, and immersive online therapy are becoming useful, particularly among those survivors who have limited physical ability to access face-toface therapy. The training of robot-assisted arms enhances specific motor skills, whereas immersive online spaces expand engagement and attention during the sessions. Immersive online environments and virtual reality platforms are increasingly used to simulate real-world tasks, expand patient engagement, and provide robust feedback during therapy sessions. These technologies help bridge gaps due to distance, resource constraints, and individual limitations.10,11
Barriers to rehabilitation: Several significant barriers prevent effective stroke rehabilitation. Stroke survivors and caregivers report that the quality of available services is not adequate. There are barriers to rehabilitation such as limited resources (especially in resource-limited areas), inadequate infrastructure, poor quality of services, unavailable rehabilitation staff, high costs and geographical disparities. There are also gaps in continuity of care beyond the initial months after stroke in most healthcare networks. Lack of information and awareness regarding stroke and stroke rehabilitation services was highlighted as a significant barrier to access among stroke survivors and their families.12
Relationships and Social Reintegration
Stroke increasingly affects the personal and community relationships of the survivors, which changes the arrangement of the house and social interaction.
Family and caregiving dynamics: Family relations have a pivotal role in the recovery process of stroke survivors. Survivors experience a shift from selfreliance to the necessity of being helped with routine chores and in family roles. Caregivers often face emotional strain, stress and financial strains. This can cause a strain in marital relationships, but in other cases, caregiving could even make relationships stronger as a joint will to power is built.13 When families actively participate in caregiving and rehabilitation, survivors experience enhanced emotional adjustment and motivation, which leads to better results and quality of life. In contrast, dysfunctional family dynamics — characterised by poor communication, unresolved disputes, or an overwhelming caregiver burden — can impede recovery, resulting in higher psychological distress, less therapy involvement, and slower rehabilitation progress.
Intimacy and relationships: Complications after a stroke often disrupt closeness, physical intimacy, and partner communication. Survivors have identified the difficulty in expressing love and sustaining past patterns of relationships.15 Professional advice and open discussion aid in improving relationship quality. Social support, affection, and open discussions are protective mechanisms, and patients who maintain strong social and emotional networks after stroke report improved relational satisfaction. A large amount of recent evidence has been released proving the critical significance of sexual function restoration to be as crucial to functional recovery as any other aspect in the context of rehabilitation.16
Community and social reintegration: Reintegration of patients after an episode of stroke into normal living is synonymous with their functional status, which is the individual's average daily performance. Community support markedly enhances post-stroke social reintegration by facilitating recovery across physical, psychological, and social domains. Survivors complain of feeling isolated because of loss of jobs, moving around or difficulty in speaking. Mutual support networks, local programs, social support from friends, family, and the local community also mitigate their isolation and help foster motivation, which not only helps manage depression and anxiety but also empowers survivors to resume meaningful social roles and relationships.17
Resilience in Stroke Survivors
A key factor in long-term stroke healing is resilience, which refers to the ability to “bounce-back” and to adjust constructively in the face of difficulty. Resilience, as opposed to the professional emphasis on functional recovery, places more emphasis on psychological and social adaptability, assisting survivors and caregivers in reestablishing fulfilling lives despite ongoing difficulties.
Psychological factors: Survivors who are more hopeful, tolerant, and confident about their abilities experience better life satisfaction. Optimism, adaptive confrontation coping, and maintaining a sense of humour help patients adjust better to post-stroke challenges and support active participation in rehabilitation, while anxiety and depression can undermine resilience and slow recovery. When a stroke patient experiences difficulties, familial and social support might help him or her re-adjust or restore the balance of physical and mental health.18
Role of social support: Survivors who have good relationships with family and their peers have favourable coping skills, motivation, and fare well when reintegrating into the community. Social support serves as a buffer to stress and promotes resilience. Changes in relationships with spouses and children have a deep impact on both patients and caregivers.19 High levels of social support are closely linked to faster and more complete functional recovery after a stroke. Studies suggest that patients with robust support systems had considerably higher increases in daily living skills and independence than those with minimal support, regardless of the initial severity of the stroke (Figure 3).20
Faith and purpose discovery: It is the religious beliefs, personal meaning, and rebuilding story that are important in strength development. Research has also revealed that caregivers who attempted positive religious coping measures had better relations with stroke survivors, and a lower level of depression was observed. More favourable responses are shown by stroke victims who view stroke as a challenge and not a result.21

Figure 3: Stroke survivor support model.
Source: Conceived and guided by Dr. Abhishek Dixit, prepared by Anushka Khatana.
Healthcare Systems and Policy Perspectives
The structure of the healthcare system has a great impact on recovery outcomes.
Disparities in access: Disparities in access to stroke therapy are primarily driven by socioeconomic inequality, with lower-income patients facing considerable disadvantages throughout the rehabilitation process. The poor survivors have a lower chance of receiving comprehensive or protracted care. The resulting cycle of disability, dependency, and medical impoverishment highlights the need for targeted policy reforms, such as subsidised services, expanded healthcare infrastructure, and equityfocused innovations like tele-rehabilitation, to bridge this gap and promote just outcomes for all stroke survivors.
Integrated care models: Evidence-based research indicates the benefits of multidisciplinary teamwork of physical therapists, occupational specialists, mental health professionals, and social workers to meet the physical and emotional needs of post-stroke patients. Recent systematic reviews and meta-analyses show that integrating these varied disciplines improves patients' health-related quality of life, allows improvements in everyday activities, and reduces depressive symptoms. Furthermore, integrated care frameworks that include both health and social care services promote long-term reintegration into home and community settings, improve caregiver support, and lower total healthcare costs.
Policy implications: Long-term care, assistance programs available to caregivers, and remote healthcare provision have to be sustained. Community-based policies that reinforce reintegration and peer networks have also been found to be effective in minimising the caregiver burden and enhancing the independence of survivors. Policies that promote community reintegration not only improve survivors' functional outcomes but also their emotional well-being by facilitating social connectedness and meaningful participation. Paid family and medical leave regulations, tax incentives for caregiving expenses, and the inclusion of informal caregivers as active partners in care delivery all guarantee that caregivers have the support, education, and resources they need to effectively handle complicated care demands.
Future Directions
Several promising trends can shape post-stroke treatment in the future:
Personalised rehabilitation using AI: Machine learning may be used to improve treatment plans to monitor patient progress and, based on the results, generate personalised and dynamic recovery paths.
Neuroregeneration and pharmacological interventions: Advances in neuroscience are examining medications and cell-based methods that have the potential to spur neural repair and enhance recovery.
Digital and virtual platforms: Immersive technology, monitoring devices, and game-based rehabilitation have great promise to enhance engagement and reach, especially in underserved groups.
Community-based resilience programs: Structured resilience-building programs, teaching mindfulness, and peer support might be beneficial to the traditional therapeutic methods.
Global policy innovation: Models that would incorporate hospital care, community rehabilitation, and caregiver support would help reduce inequalities and enhance international outcomes.
Discussion
Stroke recovery is not an easy process. It entails medical, psychological, and even social elements. Recovery programs cannot be effective without supportive relationships and strength-building strategies, and are needed to restore their functioning. There are significant changes in relationships among the survivors, and their emotional stress may increase or decrease depending on family support. Personal, social, and system-level factors all influence resilience development. However, challenges such as disproportional access to rehabilitation, disrupted healthcare services, and a lack of caregiver support curtail recovery outcomes. New innovations, particularly those based on machine learning, digital health solutions, and treatments grounded in resiliency, can help to fill these service gaps. The decision-makers are encouraged to focus on long-term models of care that extend beyond hospital stays in an emergency to the daily life of the survivors.
Conclusion
Life after a stroke is a life-long process that has its challenges and yet presents opportunities to adjust and survive. The functions of rehabilitation are restorative, relationships offer emotional and social support, and resilience enables survivors to seek sense and purpose amidst adversity. Healthcare systems and policies should evolve to encourage holistic and long-term recovery. Integrating medical and psychosocial methods with the systemic methods will help society to ensure that the stroke survivors are not only surviving but also doing well in life after the stroke.
No comments:
Post a Comment