How long will your incompetent? doctor and hospital take to get human testing going?
Do you prefer your doctor, hospital and board of director's incompetence NOT KNOWING? OR NOT DOING?
Combined therapy of focused ultrasound and aducanumab induces neurogenesis and decreases of beta-amyloid plaques in a mouse model of Alzheimer’s disease August 2022
And this from July 2018:
Ultrasound Could Help Improve Dementia Symptoms July 2018
And this from December 2021:
Using Micro-Ultrasound to Investigate the Effectiveness of Short-Term Rehabilitation following Focal Ischemic Stroke December 2021
Alzheimer’s breakthrough uses ultrasound technology March 2015
ultrasound (69 posts to March 2012)
The latest here: which your 'professional' won't know about
Sound waves stimulate stroke recovery in mice
At a Glance
- Researchers used high-frequency sound waves in mouse models of stroke to clear away harmful cellular debris and improve outcomes.
- This noninvasive approach might be used to more safely and quickly treat people with strokes caused by burst blood vessels.
Each year nearly 800,000 Americans experience a stroke. Roughly 1 in 10 strokes is caused by a burst blood vessel in the brain, known as a hemorrhagic stroke.
Hemorrhagic stroke and certain other neurological conditions disrupt the flow of a substance called cerebrospinal fluid (CSF), which helps to clear waste products and other debris from the brain. When CSF circulation through the brain declines, damaged cells and toxic substances build up. This leads to inflammation that kills neurons.
There are no FDA-approved drugs that help CSF clear more debris from the brain. And surgical treatment of stroke is invasive and must be performed in specialized medical centers. Transporting patients to those locations can delay treatment and limit access. Early nonsurgical interventions to boost CSF clearance could improve stroke outcomes.
Previous research has shown that high-frequency sound waves, commonly known as ultrasound, can help CSF clean out the brain. An NIH-funded research team at Stanford University School of Medicine, led by Dr. Raag D. Airan, studied the effects of ultrasound in the brain after stroke. Their results were published on November 10, 2025, in Nature Biotechnology.
The scientists applied their ultrasound technique to two mouse models of hemorrhagic stroke. One simulated a type of brain bleeding called a subarachnoid hemorrhage, marked by bleeding between the brain and the thin tissues that protect it. The other mimicked a type of bleeding called an intracerebral hemorrhage (ICH), marked by bleeding into brain tissues.
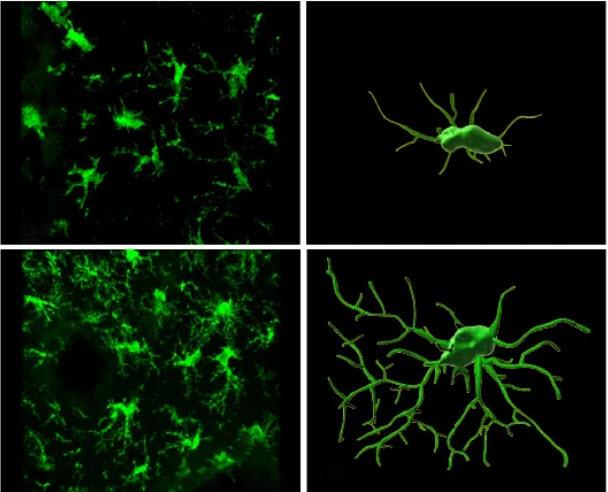
In both models, ultrasound treatment improved the clearance of accumulated red blood cells and reduced neuron death. The treatment also diminished inflammatory responses by two types of immune cell. In one of those cell types, known as microglia, ultrasound treatment increased molecular and cellular markers that suggested the cells were more engaged in clearing out unwanted material and less likely to promote inflammation.
The ICH mice showed behavioral and physical signs of impaired brain function, but the other mice did not. The ultrasound treatment reduced the ICH animals’ impairments compared to untreated ICH mice. The treated mice also had less brain swelling. Two weeks after brain injury, more than 80% of treated mice were still alive, compared to only half of untreated mice.
For comparison, the researchers then treated some of the mice with a drug that has been shown to improve CSF circulation in the brain. The drug did not increase removal of accumulated red blood cells in the brain, and these mice were more likely to die than untreated mice. This suggests that the ultrasound treatment may be safer and more effective than drugs that produce similar effects.
Protein channels that are activated by vibration or pressure played a critical role in the ultrasound treatment’s effects. When the researchers gave the ICH mice a drug that prevents activation of those proteins, ultrasound treatment no longer improved removal of red blood cells from the brain.
The results suggest that ultrasound treatment can improve debris clearance from the brain following a hemorrhagic stroke. If human studies show similar results to the mouse research, ultrasound may one day help people get stroke treatment more quickly, safely, and effectively. The approach might also be used to treat other neurological conditions that impair CSF clearance of harmful debris. This could include traumatic brain injuries.
"Ultrasound gives us access to the biology the brain uses to clean CSF," Airan says. "It lets us tune the brain’s immune system in a naturalistic way.”
No comments:
Post a Comment