It's been 8 years, has your stroke hospital done ONE DAMN THING with this? How long will you allow incompetency to last? Your stroke hospital president must think forever is the correct answer. So call your stroke hospital president and ream her/him out for not solving stroke. Point to all the research I list that has never been followed up on. What did your research analyst do with those 1400 papers in 2012? If your hospital doesn't have a research analyst reading and applying research to help stroke survivors, then you don't have a functioning stroke hospital.
Non-invasive brain stimulation in neurorehabilitation: local and distant effects for motor recovery
Sec. Brain Imaging and Stimulation
https://doi.org/10.3389/fnhum.2014.00378
- 1Human Cortical Physiology and Neurorehabilitation Section, National Institute of Neurological Disorders and Stroke, NIH, Bethesda, MD, USA
- 2Department of Medicine, Surgery and Neuroscience, University of Siena, Siena, Italy
- 3Center for Neuroscience and Regenerative Medicine, Uniformed Services University of Health Sciences, Bethesda, MD, USA
Non-invasive brain stimulation (NIBS) may enhance motor recovery after neurological injury through the causal induction of plasticity processes. Neurological injury, such as stroke, often results in serious long-term physical disabilities, and despite intensive therapy, a large majority of brain injury survivors fail to regain full motor function. Emerging research suggests that NIBS techniques, such as transcranial magnetic (TMS) and direct current (tDCS) stimulation, in association with customarily used neurorehabilitative treatments, may enhance motor recovery. This paper provides a general review on TMS and tDCS paradigms, the mechanisms by which they operate and the stimulation techniques used in neurorehabilitation, specifically stroke. TMS and tDCS influence regional neural activity underlying the stimulation location and also distant interconnected network activity throughout the brain. We discuss recent studies that document NIBS effects on global brain activity measured with various neuroimaging techniques, which help to characterize better strategies for more accurate NIBS stimulation. These rapidly growing areas of inquiry may hold potential for improving the effectiveness of NIBS-based interventions for clinical rehabilitation.
Introduction
Stroke is a leading cause of serious long-term adult disability around the world. Recovery of motor function remains highly variable despite standardized rehabilitation programs (Kwakkel et al., 2003; Go et al., 2013). The study of the mechanisms underlying recovery of motor function after stroke has been difficult due to the heterogeneity among individual lesion profiles, the severity of motor impairment and the differences in plasticity processes depending on the time passed since the ictal event.
Non-invasive brain stimulation (NIBS) has been explored as a possible technical adjuvant of customarily used neurorehabilitative treatments. NIBS, which employs electrical or magnetically-induced currents to stimulate the brain through the scalp, can temporarily excite or inhibit activity in target brain regions. In this review, we first introduce the use of NIBS in basic science and clinical neuroscience, focusing on the two most commonly used NIBS techniques (transcranial magnetic stimulation, TMS, and transcranial direct current stimulation, tDCS). We then delve into recent work exploring the effects of local application of NIBS on activity under the stimulating site and in distant brain regions. We discuss the evidence for the application of NIBS techniques in motor rehabilitation and provide a map of possible future research directions, including the combined use of NIBS with neuroimaging techniques, and the use of transcranial random noise stimulation and transcranial alternating current stimulation, among others.
Background
Early studies of “therapeutic electricity” can be traced back to the late 1800s. Since then, NIBS applications have been used in a variety of settings (for reviews, see Priori, 2003; Wagner et al., 2007a,b; Schlaug and Renga, 2008). Scientific research and public awareness of these techniques has increased greatly over the last few decades. While only a handful of papers were published on the topic in 1988, almost 1400 papers were published in 2012 alone (see Figure 1).
 Sook-Lei Liew
Sook-Lei Liew Emilliano Santarnecchi
Emilliano Santarnecchi Ethan R. Buch
Ethan R. Buch Leonardo G. Cohen
Leonardo G. Cohen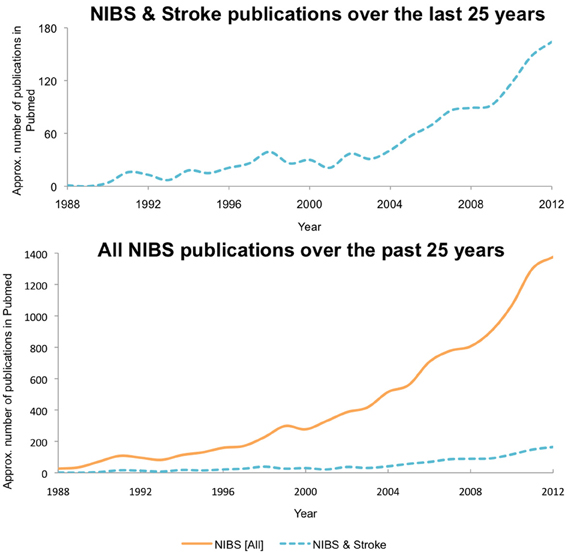
No comments:
Post a Comment