You'll have to ask your doctor and stroke hospital if this ever made it to human testing. Because with just a few modifications with nanosensors we could listen in on individual neuron signals and figure out EXACTLY what happens during neuroplasticity. Assuming of course that there is anyone in stroke research that has two neurons to rub together for a spark of innovation.
nano-sensors (3)
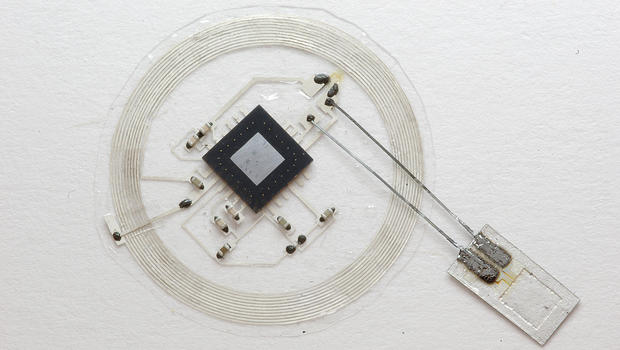
Tiny implanted sensors monitor brain injuries, then dissolve away
"This is a new class of electronic biomedical implants," Rogers said in the release. "These kinds of systems have potential across a range of clinical practices, where therapeutic or monitoring devices are implanted or ingested, perform a sophisticated function, and then resorb harmlessly into the body after their function is no longer necessary."
Rogers stressed that the technology now used for monitoring after traumatic brain injuries or brain surgery can be dangerous for patients. Systems involve bulky wires that restrict patients' movements, and invasive implants may lead to brain hemorrhages, allergic reactions, and infections.
By contrast, the tiny dissolvable silicon devices that Rogers' team developed are smaller than a grain of rice. They are naturally biodegradable -- built up on incredibly thin silicon sheets -- and dissolve away after a few weeks of monitoring brain activity. They melt harmlessly into the human body's own fluids, the researchers say.
These devices are sensitive to pressure levels in the intracranial fluid that surrounds the brain, and have a temperature sensor synced to a wireless postage stamp-sized transmitter that is placed on top of the skull.
So, what's the next phase? The team hopes to move toward human trials soon.
"The ultimate strategy is to have a device that you can place in the brain -- or in other organs in the body -- that is entirely implanted, intimately connected with the organ you want to monitor and can transmit signals wirelessly to provide information on the health of that organ, allowing doctors to intervene if necessary to prevent bigger problems," Rory Murphy, a neurosurgeon at Washington University who was a co-author of the paper.
No comments:
Post a Comment