Maybe there is something in here that can help stroke recovery but it's going to require someone else to create a protocol on it.
The dual function of microglial polarization and its treatment targets in ischemic stroke
- 1Department of Neurosurgery, Guangxi Medical University Cancer Hospital, Nanning, China
- 2Department of Neurosurgery, Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 3Department of Rheumatism, First Affiliated Hospital of Guangxi Medical University, Nanning, China
Stroke is the leading cause of disability and death worldwide, with ischemic stroke occurring in ~5% of the global population every year. Recently, many studies have been conducted on the inflammatory response after stroke. Microglial/macrophage polarization has a dual function and is critical to the pathology of ischemic stroke. Microglial/macrophage activation is important in reducing neuronal apoptosis, enhancing neurogenesis, and promoting functional recovery after ischemic stroke. In this review, we investigate the physiological characteristics and functions of microglia in the brain, the activation and phenotypic polarization of microglia and macrophages after stroke, the signaling mechanisms of polarization states, and the contribution of microglia to brain pathology and repair. We summarize recent advances in stroke-related microglia research, highlighting breakthroughs in therapeutic strategies for microglial responses after stroke, thereby providing new ideas for the treatment of ischemic stroke.
Introduction
Stroke is the leading cause of mortality worldwide (1, 2) with poor curative effect, high lethality, and poor prognosis. Among all types of stroke, ischemic stroke caused by the occlusion of blood vessels represents the majority (3). Previous research has indicated that brain injury is caused not only by the hematoma mass effect and potential hematoma expansion (which are the main causes of primary brain injury) but also by secondary brain injury (SBI) (4). Cerebral ischemia can lead to a series of pathological processes including excitatory toxicity, calcium overload, oxygen free radical damage, inflammatory responses, necrosis/apoptosis, and blood–brain barrier (BBB) destruction, which ultimately lead to irreparable neuronal damage (5). It is now proposed that injury after stroke is a complex pathophysiological process involving several genes and signaling pathways. The BBB is important, and its permeability appears to follow a heterogeneous pattern of different stroke stages associated with different biological substrates. In the hyperacute phase, sudden hypoxia damages the BBB, leading to cytotoxic edema and increased permeability; in the acute phase, neuroinflammatory responses exacerbate BBB damage, leading to higher permeability and subsequent risk, which can be stimulated by reperfusion therapy; and in the subacute phase (1–3 weeks), repair mechanisms, particularly neovascularization, occur. BBB leakage occurs in immature vessels, but this permeability is associated with improved clinical recovery. In the chronic phase (>6 weeks), an increase in the BBB restoration factor causes the barrier to begin to reduce its permeability (6). Manipulation of microglial polarization is a potential treatment strategy for patients with ischemic stroke, but small- and medium-sized glial cells in the potential molecular mechanisms of the polarization in ischemic stroke are still controversial. Despite the simplicity of the experiment, more work and clinical trials are needed to fully understand the mechanisms of microglial polarization (7). Evaluating the best time to intervene with microglia and monocyte/macrophage therapeutic strategies against ischemic stroke, as well as determining how to stimulate cells and to polarize their states, as well as the role of microRNAs (miRNA) and transplanted stem cells in mediating microglial activation and polarization during cerebral ischemia, are all important topics for future research (8, 9). Targeting specific miRNAs may provide major restorative therapy, and microglia-based therapy for ischemic stroke may become a future research area.
Recent studies have shown that there are still no effective therapeutic targets to improve the neurological function of patients after stroke, and potential treatment methods for SBI remain a hot point of research. Currently, an effective treatment for ischemic stroke is mainly intravenous thrombolysis and mechanical thrombectomy. However, these treatment options are limited by the recommended treatment window (10, 11). In addition, a series of reperfusion injuries caused by inflammation and oxidative stress may occur after ischemia-reperfusion (12); oxidative stress can induce inflammation (13, 14). There is increasing evidence that, during cerebral infarction, persistent neuroinflammation damages neurons and the BBB, leading to tissue destruction and impaired function (15–17). Neuroinflammation plays a crucial role in ischemic stroke-induced brain injury and affects disease prognosis. Future research will focus on controlling stroke-induced inflammation by targeted drugs and will be challenging.
Microglia are the permanent substantial macrophages in the central nervous system (CNS), and activated microglia typically behave “amoeba-like,” primed for action (18). Several findings showed that almost five different types of microglia morphology were identified in control and experimental status epilepticus (SE) tissues, and were categorized as follows: (1) ramified; (2) hypertrophic; (3) bushy; (4) amoeboid; and (5) rod-shaped (19) (Figure 1). Microglial polarization plays a major role in promoting brain injury and nerve recovery (20). As the main source of inflammatory cells in ischemic brain injury, microglia play a key role in the inflammatory response after stroke (21). After stroke, microglia are polarized to the classical pro-inflammatory type (M1-like) or the alternative protective type (M2-like) under optimal conditions (8). Classical M1-like microglia are related to the induction of pro-inflammatory molecules, while other M2-like microglial activations are related to neuroprotection (22). In this review, advances in microglia and ischemic stroke, including the dual functions of phenotypic polarization of microglia/macrophages and polarization-related signaling pathways, have been studied. Future ischemic stroke treatments may target microglial polarization in the future.
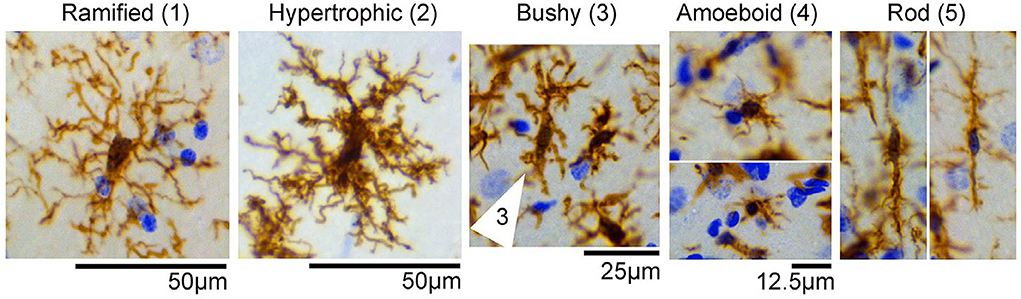
Figure 1. Representative images of microglial/macrophage cells (brown) with different morphologicalphenotypes observed in the control and status epilepticus (SE) groups, including (1) ramified, (2) hypertrophic, (3) bushy (cell indicated by arrows), (4) amoeboid, and (5) rod-shaped. Images were taken from the hippocampus of control or SE animals. Nissl-stained nuclei are indicated in blue [the figure is reproduced (19)].
Origin and function of microglial cells
Derived from primitive yolk sac progenitor cells, microglia are a type of fixed macrophages (9). The number of microglia showed a steady increase in the first 2 weeks after birth, and gradually decreased to 50% of the level at birth between 3 to 6 weeks later, after which the density gradually stabilized. A decrease in the rate of proliferation accompanied by an increase in apoptosis results in a decrease in the overall number of microglia, and mature microglia maintain their numbers in the CNS by self-renewal (23, 24). In the CNS, microglial cells in the brain of healthy adults are renewed to maintain their number and local expansion (25). In the physiological state, microglial cells present a typical branch-like state of small cell body and long branches and are referred to as “resting microglial cells.” The protrusions have high mobility and can carry out extensive and continuous monitoring of the surrounding environment. In the pathological state, microglial cells are changed from the resting state to the active state. Polarization refers to the fact that microglia are affected by exogenous substances to achieve a specific phenotype, and there are one or more molecular markers and significant changes in molecular distribution (26). M1-like and M2-like microglia are essential in tissue damage and repair, respectively. Polarization of M1-like and M2-like microglia is also considered a functional manifestation of CNS disease, which is specifically manifested in the release of CNS disease-related inflammatory factors and the role of neuroinflammatory responses (27–29).
More at link.
 Yong Mo
Yong Mo Weilin Xu
Weilin Xu Kaijing Fu
Kaijing Fu Hainan Chen1,
Hainan Chen1,  Ligen Mo
Ligen Mo Jun Yan
Jun Yan
No comments:
Post a Comment