Since this was not tested on stroke individuals it is the responsibility of your stroke doctors and hospital to get it tested in stroke patients. What ankle exoskeleton is already in use in your rehab department? Nothing? Then why is it even considered a stroke department?
Usability and performance validation of an ultra-lightweight and versatile untethered robotic ankle exoskeleton
Journal of NeuroEngineering and Rehabilitation volume 18, Article number: 163 (2021)
Abstract
Background
Ankle exoskeletons can improve walking mechanics and energetics, but few untethered devices have demonstrated improved performance and usability across a wide range of users and terrains. Our goal was to design and validate a lightweight untethered ankle exoskeleton that was effective across moderate-to-high intensity ambulation in children through adults with and without walking impairment.
Methods
Following benchtop validation of custom hardware, we assessed the group-level improvements in walking economy while wearing the device in a diverse unimpaired cohort (n = 6, body mass = 42–92 kg). We also conducted a maximal exertion experiment on a stair stepping machine in a small cohort of individuals with cerebral palsy (CP, n = 5, age = 11–33 years, GMFCS I-III, body mass = 40–71 kg). Device usability metrics (device don and setup times and System Usability Score) were assessed in both cohorts.
Results
There was a 9.9 ± 2.6% (p = 0.012, range = 0–18%) reduction in metabolic power during exoskeleton-assisted inclined walking compared to no device in the unimpaired cohort. The cohort with CP was able to ascend 38.4 ± 23.6% (p = 0.013, range = 3–132%) more floors compared to no device without increasing metabolic power (p = 0.49) or perceived exertion (p = 0.50). Users with CP had mean device don and setup times of 3.5 ± 0.7 min and 28 ± 6 s, respectively. Unimpaired users had a mean don time of 1.5 ± 0.2 min and setup time of 14 ± 1 s. The average exoskeleton score on the System Usability Scale was 81.8 ± 8.4 (“excellent”).
Conclusions
Our battery-powered ankle exoskeleton was easy to use for our participants, with initial evidence supporting effectiveness across different terrains for unimpaired adults, and children and adults with CP.
Trial registration Prospectively registered at ClinicalTrials.gov (NCT04119063) on October 8, 2019.
Background
Ankle exoskeletons hold potential to augment walking performance in unimpaired individuals and in individuals with neurological conditions [1,2,3,4]. The ankle joint is a frequent target for powered assistance due to its critical role in efficient bipedal locomotion [5,6,7] and because it is a commonly affected joint in individuals with neurological deficits [8, 9]. Individuals with cerebral palsy (CP), for example, typically have ankle plantarflexor weakness and limited push-off power that contributes to slow, inefficient walking, particularly on graded terrain, like stairs [10,11,12].
Unburdened by the need to carry motors and a power supply, users walking with tethered ankle plantarflexor assistance have consistently demonstrated improved walking economy for nearly a decade [7, 13,14,15]. However, achieving improvements in walking economy with untethered ankle exoskeletons has apparently been more challenging, with only a small number of studies reporting activity performance benefits compared to walking without the device [1, 3, 16,17,18]. Untethered ankle exoskeletons capable of mobility augmentation outside of the laboratory follow two general design approaches: placing motors on the shank close to the joint or placing motors at the waist. Opting to minimize mass and the physical profile added to the lower-limb, Awad et al. [1, 17] developed a soft exosuit with waist-mounted motors that improved paretic limb function, walking speed and walking economy in stroke survivors. Mooney et al. [3] took a shank mounted motor approach instead, and addressed the metabolic detriment of adding mass distally on the leg by incorporating a clever mechanical design achieving high torque and power output, and demonstrated improvements in loaded and unloaded walking in healthy adults; this appears to be the only published work demonstrating a group-level improvement in energy efficiency in unimpaired individuals when walking with an untethered, battery-powered ankle exoskeleton compared to no device.
For several years, our group has worked on untethered, low-torque ankle exoskeletons for children and young adults with CP. We have demonstrated that bilateral assistance proportional to the user’s biological ankle moment during stance phase [19, 20] can improve key metrics such as energy expenditure and walking speed in small cohorts with CP during level walking [18, 21]. However, early prototypes had poor reliability and durability, and proved ineffective for individuals of body mass greater than approximately 45 kg because of limited torque production and significant motion of the ankle assembly relative to the shank and foot. Additionally, these prior exoskeletons were cumbersome to don and doff, designed without consideration for usability, and control was limited to a computer-based researcher interface. Usability factors are important yet under-researched aspects of wearable lower-limb exoskeleton design that hold practical implications for real-world deployment. Devices intended to augment mobility in the community should be easy to don and operate, with portable and intuitive user interfaces. The ability of individuals with CP to put on and operate an ankle exoskeleton without researcher or technician intervention remains unknown.
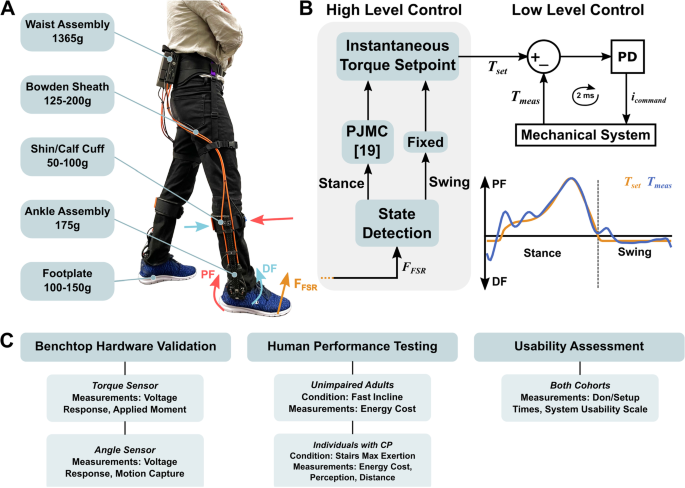
The first goal of this study was to design a novel cable-driven ankle exoskeleton, validate custom torque and angle sensors, and evaluate electromechanical performance during ambulation (Fig. 1). Our second goal was to highlight the relevance and versatility of this device by demonstrating its ability to reduce the energy cost of fast incline walking in healthy adults, and on distance achieved during a maximal exertion stair-stepping exercise in CP. We selected these moderate- to high-intensity activities for these human performance experiments because we believe such activities reflect the real utility of ankle exoskeletons in both unimpaired and impaired populations, namely, augmenting ambulatory activities that have elevated ankle plantarflexor demand. We hypothesized both cohorts would have significant improvements while walking with vs without the device. Our final objective was to complete a usability assessment, quantifying the time for users or their caretakers, if applicable, to don and set up the device without researcher intervention. We hypothesized that individuals could don, calibrate, and receive assistance from the device in less than 5 minutes.
Exoskeleton mass breakdown, exoskeleton control overview, and protocol summary. A Device components and mass. Values are mass per leg except for the waist assembly. B High- and low-level control layers. The high-level controller was responsible for gait event detection (i.e., toe-off and heel strike) and assistive torque profile generation. During stance, a forefoot force sensor signal was an input to a proportional joint moment controller (PJMC) that generated an adaptive plantarflexor torque profile in real time [17]. During swing, a constant dorsiflexor torque was prescribed. The low-level controller tracked the plantarflexor and dorsiflexor torque profiles using a closed-loop PD controller. C A summary of the experiments, cohorts, conditions, and measurements analyzed in this study
No comments:
Post a Comment